Patterns of Misdiagnosis in Plain Film Radiography
Introduction
Misdiagnosis in plain film radiography is not an uncommon event. The Red Dot system was largely developed as a response to plainfilm misdiagnosis and its associated legal costs in a hospital in the UK (see BMJ 1985: 290 : 421-422). The causes for the most common misdiagnoses tend to fall into a few categories. An awareness of these causes can assist in avoiding repetition of errors.
Categories of Misdiagnosis
The following are common categories of causes of misdiagnosis in musculoskeletal plain film imaging. These groups are not mutually exclusive- a misdiagnosis may relate to several groups or none of them.
1. Normal Anatomy
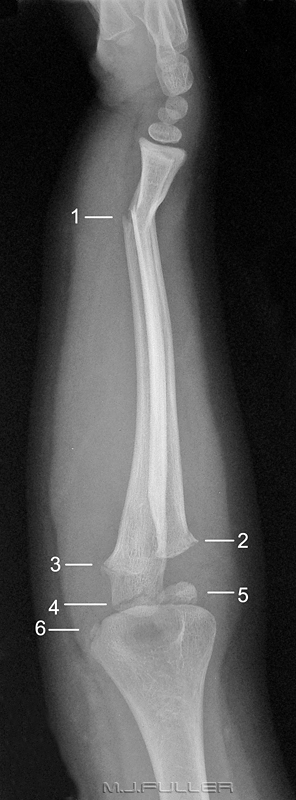
Category of Misdiagnosis Discussion 1. Normal Anatomy It is self-evident that you cannot recognise abnormal anatomy if you cannot recognise normal anatomy. This is a common cause of difficulty in diagnosis amongst junior staff 2. Normal Anatomical Variants This is very closely related to the category above. If you are not familiar with common normal anatomical variants they can easily be mistaken for pathology. Normal variants do not need to be memorised- rather, a copy of Keat's Atlas of Normal Anatomical Variants should be your department's first book purchase 3. Pattern Recognition Failure Also closely related to the above, there are common plain film pathological appearances. Once these are known, your eye is drawn to them with little effort. 4. Referral Failure The radiographer relies on the referring doctor to request the correct anatomy- pathology not imaged is pathology not recognised 5. Associated Fractures/pathology This is a failure to recognise associated pathology (sometimes referred to as comorbidities although this term is not strictly correct). This might be considered a type of referral failure or radiographer failure or both. 6. Inadequate Number of Projections The single image will rarely suffice in radiography. In some cases, the traditional two views at right angles will not suffice (how many ankle fractures are missed on a two view series?) 7. Radiography Failure This covers a variety of failures. If the images are substandard there is a risk that the diagnosis will suffer the same fate. 8. Photographic vs Clinical Radiography From the radiographer's point of view, this is arguably the big one. If you approach radiography as a photographic-like exercise, you will miss more pathology. If you consider mechanisms of injury, clinical presentation, soft tissue signs, and a variety of other indicators of pathology, you will have a higher diagnostic success rate. 9. Inclusion Failure One of the aims of the trauma radiographer should be inclusiveness.
Patients will not present with injuries that fit neatly into the radiographic anatomical regions that you have been taught to image10. Peripherally Positioned Pathology This is closely related to the above. When pathology is demonstrated in the anatomical periphery of an image, it is more likely to be missed. 11. Unexpected/incidental findings You tend to look for pathology in the context of the patient's presentation. If you missed the bone tumour it may be because you weren't looking for it. It is better to perform a targeted search and a systematic search for pathology 12. Satisfaction Syndrome There is a well recognised tendency to miss fractures when the first fracture is identified - you cease looking when the patient's symptoms have been accounted for 13. The extremely subtle and the extremely obvious It is expected that an extremely subtle finding may be missed, but less so the blindingly obvious pathology 14. Soft Tissue signs and False Positives When investigating potential fractures, soft tissue signs are useful in avoiding false positives 15. The 'trivial' injury in multi-trauma Patients who present with multitrauma can suffer fracture diagnosis failure through a combination of time-limitation, distracting injury and trivialising of injuries perceived as less important 16. Artifacts Artifacts can both obscure pathology and mimic pathology 17. A "Fair Miss" Some fractures and dislocations were meant to be missed. That is to say, despite all fair and reasonable efforts, the fracture identification was not achievable with plain film radiography (even when evident in retrospect)
This is a problem that you encounter in the early part of your career. It is largely overcome with time- even without effort, once you have taken 1000 chest X-ray images, you start to identify abnormal anatomy with ease.
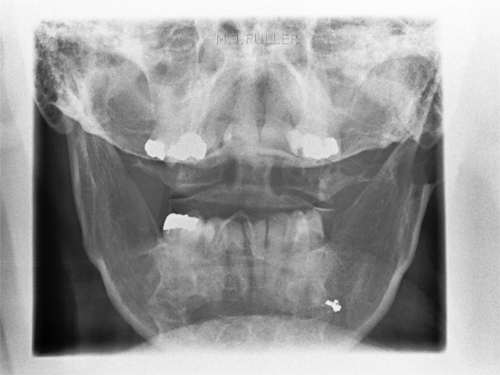
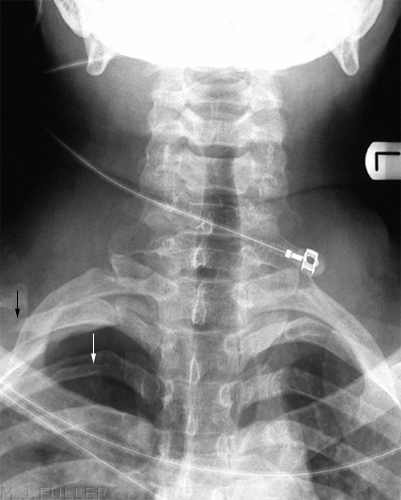
Children can present difficulties in recognising normal bony anatomy because of the complicating presence of the physis. This patient has an easily identifiable fracture of the clavicle, but what do you make of the two arrowed structures? If one of the arrowed structures is the growth plate, what is the other- is it a fracture?
The answer is no- it is a single structure, the proximal humeral growth plate, that is somewhat "V"shaped. It can appear as two structures, particularly on the internal rotation view. I have seen this appearance mistaken as a fracture twice.This image of a patient with a Salter Harris I injury to the proximal humeral growth plate may help your understanding of the anatomy. Note that when the arm is externally rotated, the growth plate takes on a vaguely V- shaped appearance.
<a class="external" href="http://www.e-radiography.net/" rel="nofollow" target="_blank">http://www.e-radiography.net/</a>
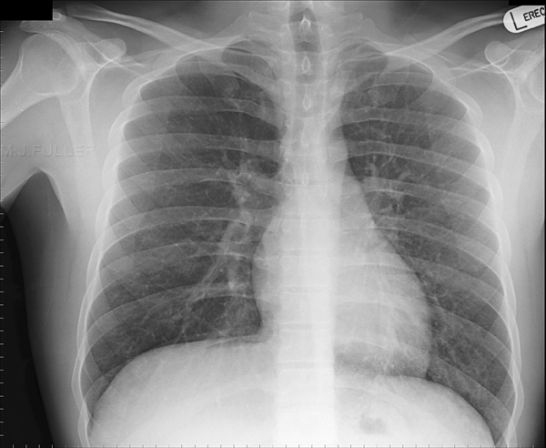
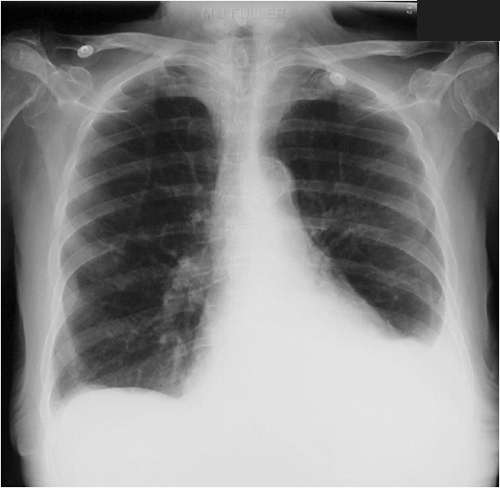
Recognising normal anatomy is a form of pattern recognition in much the same way as you learn abnormal patterns. If you view a chest image up-side-down, the pattern recognition of normal anatomy just doesn't kick in despite the fact that the information available is exactly the same as the correctly orientation image (below left). Pasteur wrote that "Chance (observation) favours the prepared mind." This is true
when interpreting X-ray images. It is much easier to read a chest radiograph
when it is right-side up than up-side down, because we are used to viewing it this way and we have a mental image of what a chest roentgenogram is supposed to look like.
adapted from <a class="external" href="http://www.hand-therapy.com/images/Radiology_100500.pdf" rel="nofollow" target="_blank">Karen Nugent, PT, CHT and David Nelson, M.D. RADIOLOGY OF THE WRIST</a>
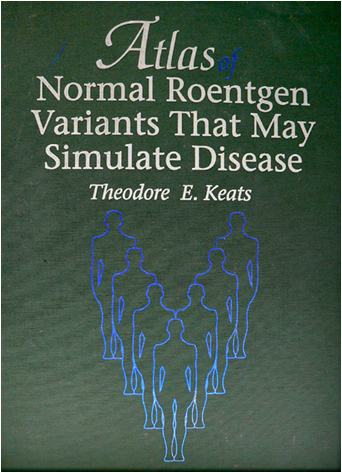
If you are not familiar with common normal anatomical variants, they can easily be mistaken for pathology.
Applying a plaster cast to a patient's ankle and leaving it there for 6 weeks is undesirable (at many levels) in a patient who has had a normal anatomical variant misdiagnosed as an ankle fracture.
When it comes to normal anatomical variants, Keat's Atlas is your best friend. Every Emergency Department that offers a plain film radiography service should have a copy of this book
3. Pattern Recognition
...there are common plain film pathological appearances. Once these are known, your eye is drawn to themThere is little doubt that plain film pathological appearances that you are familiar with are more likely to leap out of the image and punch you in the eye. You tend to quickly scan the image for all of the patterns that you know. You can't, ipso facto, look for a pattern that you don't know
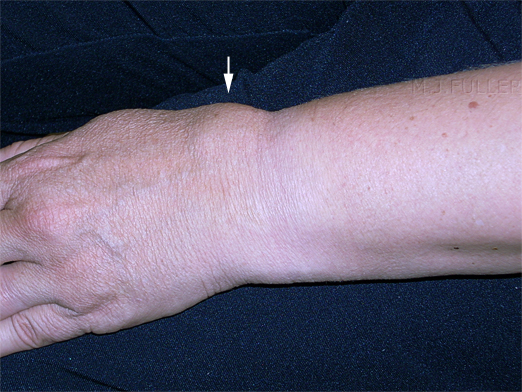
When I first saw this image there were two pathological features that struck me immediately. If this wrist looks normal to you, there are probably at least two plain film pathology patterns that you are not familiar with.
...see belowThe first is the so-called Terry Thomas sign (black arrow). This refers to the increased distance between the scaphoid and the lunate. This sign can indicate a rupture of the scapho-lunate ligament.
The origins of the term should be discernible from this photograph of Terry Thomas
The other sign is the pronator quadratus soft tissue sign (white arrow). This is a bowing of the facial covering of the pronator quadratus muscle and indicates significant injury to the wrist and a higher chance of bony injury.
(more information on the pronator quadratus sign at <a class="external" href="http://radiology.rsnajnls.org/cgi/reprint/244/3/927.pdf" rel="nofollow" target="_blank">http://radiology.rsnajnls.org/cgi/reprint/244/3/927.pdf</a>)
4. Referral Failure
If the referring doctor has not requested imaging of the correct anatomy (not views... anatomy), the diagnosis is likely to be missed.
The clinical information is also important. There is a misconception from some referring doctors that the radiography is determined by the examination requested only- often not true; it is the examination requested and the clinical information together that will guide the radiographer to perform the most appropriate projections
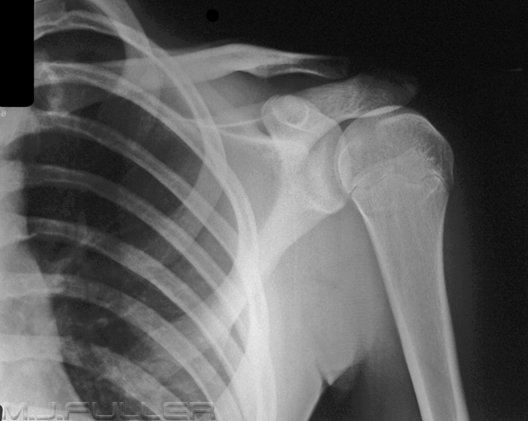
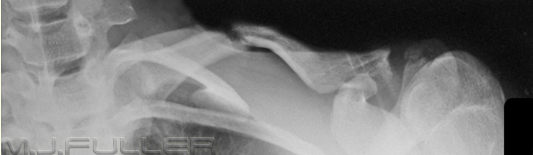
It is helpful if the referring doctor has a good grasp on clinical appearances of common pathology. The images below show classical appearances of a high grade AC joint dislocation and an anterior gleno-humeral joint dislocation. Confusing the two appearances is not likely to lead to misdiagnosis, but it isn't helpful either!
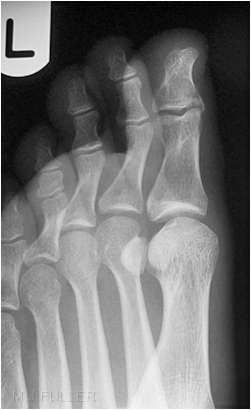
Foot and Ankle
This is the common one. Even experienced registrars in the Emergency Department have told me that they are often not sure when to order foot radiography and when to order ankle radiography. It is sometimes very difficult given that an ankle injury can present with foot symptoms. The key is the talus. If you think the injury is distal to the talus, you should ask for foot radiography. If you think the injury is proximal to the talus, you should ask for an ankle X-ray. The next question is usually "what should I ask for if I think the patient has an injury to their talus?" Answer- "talus X-ray"
Another conversation I have had in the in the Emergency Department goes like this....
Doctor: "I don't know what views to ask for with this patient" Radiographer: "Which professional group in the hospital are experts in radiographic views?" Doctor: "the Radiographers?" Radiographer: "Do you think they need advice on which views to take?" (hint of sarcasm) Doctor: "I guess not, but I still don't know what to ask for" Radiographer: "What do you want images of?" Doctor: "the talus" Radiographer: "then you should ask for X-rays of the talus... we will work the views out"
The other "Emperor's Clothes" point is that unless you (the referring doctor) are an expert on the subject, and/or the requested views make good sense, they are probably not going to be performed anyway. If they do make good sense, they would probably have been performed without asking. My view is that the person who is reporting the X-ray images gets first call at which views are performed. The referring doctor and the radiographer get to influence the final series of views depending on the circumstances of the case. The resus room situation is different.
ps I am a grumpy old radiographer
5. Associated Fractures (comorbidity)
This is sometimes a form of referral failure best illustrated by example- when a patient presents with a widened ankle mortise following trauma, there can be an associated fracture of the upper third of the fibula. Failure to recognise this association can result in a missed diagnosis of Maisonneuve fracture
6. Inadequate Number of Projections
The number of views required is the number needed to demonstrate all of the demonstratable pathology
The single projection represents a risky approach in orthopaedic plain film radiography. There is great truth in the dictum "one view is no view" (from Dr John Harris). One of the few exceptions is the survey examination where the cost-vs-yield considerations are different
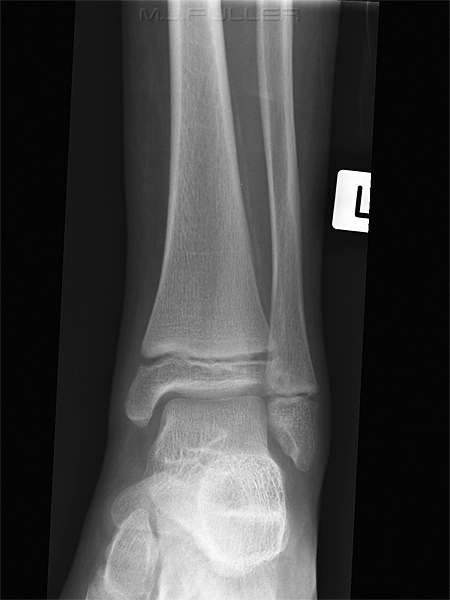
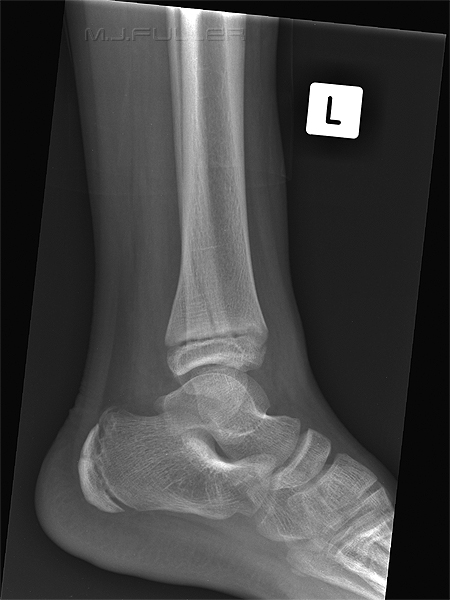
Case 1- Single View Inadequate
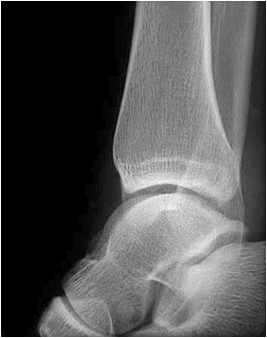
This is an AP ankle image. There appears to be no obvious fracture or dislocation.
(? visible tibial periosteum)The lateral view reveals a fibula fracture
Case 2- Single View Inadequate
This is an AP shoulder image in a patient who was referred for clavicle radiography. There is no displaced clavicle fracture seen. The dedicated clavicle view demonstrates a fracture which was not visible on the AP shoulder view
Case 3- Two Views Inadequate
Case 4- Three Views Inadequate
7. Radiography Failure
...if you thought these cases were rare...
These 2 cases have made me wary of passing a lateral ankle image where the cortex of the tibia and fibula overlap posteriorly. The lateral ankle view does not need to be very 'off true lateral' for this to occur. Fractures of the posterior malleolus of the tibia are best demonstrated on the lateral ankle image (in some cases only demonstrated on the lateral), so you may only get one chance at demonstrating this fracture on the routine views. Just to add a point of confusion, the off-lateral ankle can be a very useful supplementary view when certain types of fractures are suspected on the routine views (see posterior malleolus fractures)
Case 3
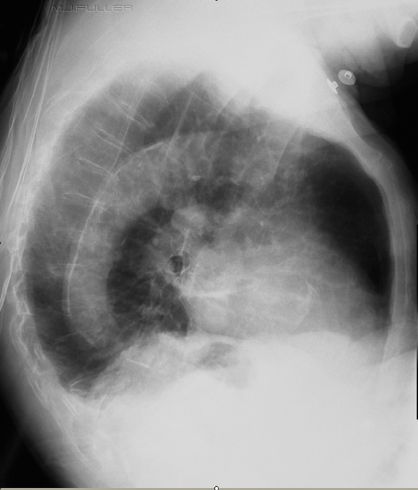
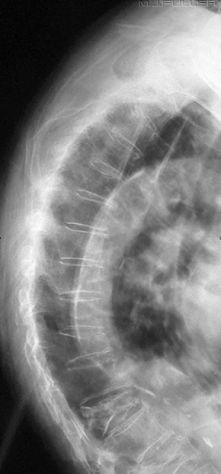
The radiographer has performed an erect PA and lateral X-ray examination using the AEC. The lateral chest image is shown below.
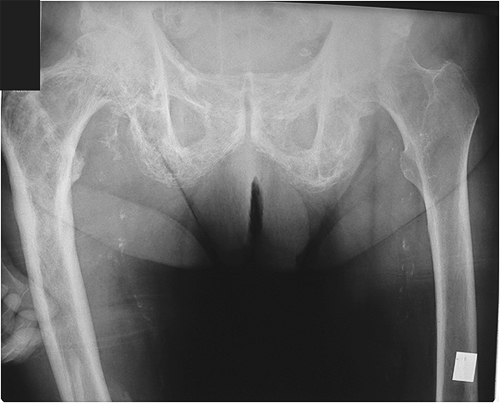
Neck of Femur Fractures
The diagnosis of neck of femur fracture is difficult if the patient's feet are not internally rotated as shown above External rotation of the feet causes the trochanters to overly the femoral neck
8. Photographic vs Clinical Radiography
9. Inclusion FailureIf you approach radiography as a purely photographic-like exercise, you will miss pathologyThis is possibly the most important determinant of missed fractures related to the actions or omissions of the radiographer. The narrow approach to radiography as a photographic-like exercise is, in my view, anachronistic. It was appropriate 30 years ago but has since been replaced by a clinical approach to radiography. The clinical approach starts with the patient and ends with the patient. The radiographer must understand why the patient has presented for imaging before the examination starts. This may require taking a brief history from the patient so that you fully understand the mechanism of injury and the patient's symptoms. The referral may describe pain, or swelling, or deformity, but until you have observed this yourself, you have no precise idea of degree, distribution etc. A musculoskeletal injury may be apparent to the radiographer before the X-ray examination begins. Furthermore, the routine images can be examined in the context of the patient's history and clinical signs. Further imaging can be undertaken following consideration of everything that you know about the patient's presentation- not just the initial plain film series.
The following case illustrates a clinical radiography approach to a patient who presented to the ED with trauma to her wrist.
Case 1This lady presented to the Emergency Department after a fall and was referred for wrist radiography. The images below show her wrist after the bandage was removed. She was in considerable pain and the focal swelling over the dorsum of her wrist suggested that she may have sustained a fractured radius.
Routine wrist views were performed
This series demonstrated no obvious fracture... although the distal radius is suspect looking. The scaphoid fat pad (white arrow) and the pronator fat pad (black arrow) were normal.
The radiographer was convinced clinically that the patient had sustained a fracture and considered whether the soft tissue signs were misleading (as there are known to be on occasions). Supplementary views were performed as shown below.
10. Peripherally Positioned Pathology...one of the aims of the trauma radiographer should be inclusiveness.
...patients will not present with injuries that fit neatly into the anatomical regions that you have been taught to image
Radiographers in the Emergency Department may suffer from a conflict between X-ray beam collimation and anatomy inclusion- you want to collimate the primary X-ray beam to minimise radiation dose to the patient but you do not want to collimate-off abnormal anatomy. One of the more common examples of this is the inclusion of the base of the 5th metatarsal on the lateral ankle view in trauma patients. Fractures of the base of the 5th metatarsal are known to be associated with inversion injuries to the ankle. If you have not assessed the base of the 5th metatarsal clinically or radiographically you may miss a fracture leading to problems of delayed union.
| A deliberate gap here! |
11. Unexpected and incidental findings
12. Satisfaction Syndrome
There is a well recognised tendency to miss fractures when the first fracture is identified
- you cease looking when the patient's symptoms have been accounted for
Case 1
13. The Extremely Subtle and the Extremely Obvious
Case 2
It goes without saying that the more subtle the pathology, the more likely that it will be missed. What is surprising is that an extremely obvious pathology can elude the observer, particularly when it is incorrectly dismissed as artefactual or a normal variant.
Case1Patient History
unknown
Images
Discussion 1
The radiographer assessed the routine views in the context of the patient's mechanism of injury and clinical features. She considered there was a reasonable possibility that this patient had sustained a fracture of the posterior malleolus of the tibia and there was a fair chance of demonstrating such a fracture by performing off-lateral views of the ankle.
Discussion 2
The Defect in the posterior cortex of the distal tibia was, by any fair assessment, a subtle finding. The radiographer performed very well in identifying this defect and performing the supplementary views which demonstrated the fracture. If the supplementary view had not been performed, the missed fracture would probably have been considered to be a fair miss.
14. Soft Tissue Signs
...absence makes the diagnosis grow stronger
Soft tissue signs in musculoskeletal plain film imaging easily get themselves a bad name because they are considered to be unreliable. My view is that they are very useful if they are considered for what they are- indicators of possible underlying bony injury. Importantly, it is not the presence of a soft tissue sign that I find most useful- it's the absence of one. Even those soft tissue signs that are notoriously unreliable (such as the scaphoid fatpad sign) can be useful in eliminating underlying fracture. For example, if there is debate as to whether a patient has a subtle scaphoid fracture, the demonstration of normal adjacent soft tissue structures (no scaphoid fatpad sign) tends to suggest that there is no scaphoid fracture.
The case below is a special case in that a lipohaemarthrosis is one of the few soft tissue signs that is a definite indicator of (articular) fracture.
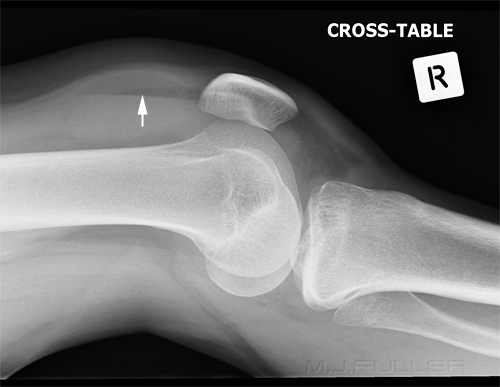
Case 1This patient presented to the Emergency Department following a sports injury the previous day. The patient sustained a blow to the knee and is now UTWB and is in great pain. The initial AP and lateral knee images are shown below
The Radiographer has performed AP and lateral horizontal ray views as shown above. There is evidence of a lipohaemarthrosis on the lateral image (white arrow). The fat/blood interface is not seen sharply. The radiographer decided to repeat the lateral view to try and confirm the presence of a lipohaemarthrosis.
The lipohaemarthrosis is now clearly seen. (the reason for the improved visualisation of the fat/blood interface on this repeat view is unclear)
The confirmation of the lipohaemarthrosis indicates that the patient does have a fracture that involves the knee joint. Given that the site and nature of the fracture had not been firmly demonstrated, the radiographer proceeded to perform oblique views of the knee.
The external oblique image clearly demonstrates a tibial plateau fracture of the lateral tibial condyle (white arrow).
15. The "Trivial" Injury in Multitrauma
through a combination of time-limitation, distracting injury and trivialising of injuries perceived as less important
I was advised by an ICU staff member that followup on former ICU multi-trauma patients can reveal some surprising results. One of the patterns of long-term effects is from missed fractures and dislocations that were considered low priority at the time. This is understandable in a resus situation where concerns of keeping an airway open or dealing with a pneumothorax will take priority over the possibility of a dislocated thumb. When patients are asked about long-term effects of their injuries at follow-up (12 months after their discharge from ICU) it can be the discomfort from the missed dislocated thumb that causes the greatest impact on their quality of life. I am mindful of this when working in the resus room. If the patient is waiting to go to CT or waiting to go to theatre or ICU it is worth examining the patient's limbs carefully for evidence of fractures and dislocations.
16. Artifacts
17. The Plain Film "Fair Miss"
That is to say, despite all fair and reasonable efforts, the fracture identification was not achievable with plain film radiography
Despite the best intentions of all staff involved, fractures and dislocations are missed. They are typically revealed on subsequent plain films, MR, CT or Nuclear Medicine imaging. With the advent of MR imaging, it is clear that some fractures are present at the time that the plain film image was acquired but need MR imaging to be demonstrated. The scaphoid fracture and the neck of femur fracture are some of the more common cases.
A slightly different case of the fair miss is the plain film fracture that is only visible through the 'retrospectoscope'. That is, an appearance on plain film that could not reasonably be commented on as a possible fracture, but is revealed to have represented a fracture on subsequent imaging.
Summary
There is considerable overlap between the categories of misdiagnosis considered above. Failure to perform a supplementary view of a patient's ankle when there is suspicion of undemonstrated fracture suggests a photographic approach to radiography. It could also be considered to be an inadequate number of views and/or satisfaction syndrome if another fracture had already been demonstrated. It is no longer acceptable for radiographers to say "... don't blame me... I just take the pictures". The radiographers work as part of the clinical team and must shoulder responsibility for missed pathology where it was within their scope of practice to perform the views necessary to demonstrate the pathology.
back to the Applied Radiography home page