Wrist Arthrography
Introduction
A wrist arthrogram is a radiographic /fluoroscopic examination of the wrist joint(s) following the injection of a contrast agent into the wrist joint cavity or cavities.
The Wrist Joint Compartments
Wrist arthrography requires opacification of three separate compartments which do not intercommunicate in the normal wrist. These compartments are
- The Radiocarpal
- The midcarpal
- The distal radio-ulnar joint
Indications
"The major indication for wrist arthrography is to demonstrate preoperatively the presence of a clinically suspected tear or defect in one of the connecting structures [intercarpal ligaments and capsule attachments]. Tears or defects are confirmed when communication between normally noncommunicating compartments is demonstrated. (Gilula, L.A. The Traumatised Hand and Wrist, Radiographic and Anatomic Correlation,, 1992, p14).
Contra-indications
- non-consent by patient to procedure
- contrast media or iodine allergy
- pregnancy (risk is minimal but patient may wish to delay procedure)
Objectives
Wrist athrography may be undertaken to
- outline wrist ligaments to determine their structural integrity.
- preoperative anatomy assessment
Technique
Preparation
- patient identification (3 'C's- correct patient, correct side, correct procedure
- completed consent form
- no diet restrictions
- collect/retrieve/collate relevant previous imaging for ease of review prior to procedure
Wrist Injection
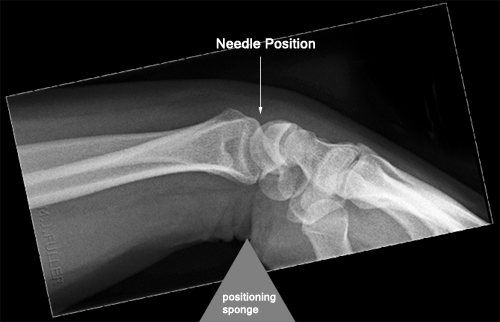
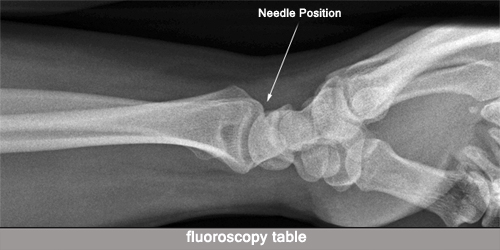
The injection off contrast into the wrist joint should be undertaken as a sterile fluoroscopic procedure. The patient can be seated at the end of the fluoroscopy table with his/her wrist resting on the fluoroscopy table. Alternatively, the patient can be lying prone on the fluoroscopy table with his/her affected wrist in a PA position above his/her head. A small triangular (or similar) positioning sponge is placed under the patient's wrist to cause the patient's wrist to be in a stable/comfortable flexed position. This position will profile the radioscaphoid joint- the ideal size of the triangular sponge will depend on the patient's palmar tilt (0 - 20 degrees but more commonly 10 - 15 degrees). Alternatively, the injection may be made slightly distal to what appears to be the radioscaphoid joint, and the needle angled toward the elbow to match the palmar tilt. In anxious patients, where there is a moderate to high risk of the patient fainting, the patient would arguably be more safely positioned on the the fluoroscopy table in a prone position with his/her affected arm above his/her head.
The injection site should be selected with a view to avoiding injecting at the site of probable abnormality. This will avoid any extravisated contrast obscuring the anatomy of interest. The normal site is the dorsal radioscaphoid region.
Carpometacrapal joint 2 - 5 are usually filled with the midcarpal injection. A fourth compartment, the pisotriquetral joint, communicates with the radiocarpal joint in 3/4 of patients. A fifth compartment, the first carpometacarpal joint, is a separate compartment, and its opacification indicates an abnormal communication. "The major indication for wrist arthrography is to demonstrate preoperatively the presence of a clinically suspected tear or defect in one of the connecting structures [intercarpal ligaments and capsule attachments]. Tears or defects are confirmed when communication between normally noncommunicating compartments is demonstrated. (Gilula, L.A. and Totty W.G. in The Traumatised Hand and Wrist, Radiographic and Anatomic Correlation,, 1992, p14).
Contrast is injected until the patient experiences discomfort from the increased pressure in the wrist joint compartment.
Positioning for the other wrist compartment injections is achieved with the wrist placed flat on the imaging table. Modification of the wrist position may be required to profile the joint to be injected. Continuous fluoroscopy during injection is required to identify the early passage of contrast material though damaged ligamentous structures. Repeat images after wrist exercise may help to force contrast through very small tears in damaged ligamenst.
Imaging
Radiographs or digital spot images (DSI) should be taken in the AP/PA, lateral and oblique positions. Additional projections may be useful depending on the anatomy of interest. Fluoroscopy during contrast injection is highly desirable. Identification of a ligament defect/tear/abnormal communication is easier if you see the contrast passing through an abnormal communication.
The Radiocarpal Joint
<embed height="300" src="http://widget.wetpaintserv.us/wiki/wikiradiography/widget/genericvideo/68624b605b94e26375f28f521682a996d023b7ca" type="application/x-shockwave-flash" width="300"/>
Pathology
The most common sites of abnormal communication are, in order
- the scapholunate ligament
- the lunotriquetral ligament
- the triangular fibrocartilage
(Gilula, L.A. and Totty W.G. in The Traumatised Hand and Wrist, Radiographic and Anatomic Correlation,, 1992, p14).