Radiation Safety
Jump to navigation
Jump to search
Radiation protection is an important consideration due to the potential for ionization radiation (x-rays) to disrupt the molecular structure of organic cells, which may result in functional impairment of tissues and organs. The potential damage is related to the exposure, the duration of exposure and the area of tissue exposed.
These are the three cardinal rules of dose reduction and radiation safety
Time - refers to the length of exposures, in that shorter exposures will produce less radiation dose. This can be controlled by reducing the mAs used in general radiographic practice and minimising the screening time in fluoroscopy. Halve the time, halve the dose.
Distance - refers to the distance between an individual and the radiation source (eg the X-ray tube). This is the most effective method of minimising dose to staff members, even small increases in distance can result in significant dose reductions. Double the distance, quarter the dose.
Shielding - refers to both fixed protective barriers and personal protective equipment, such as lead gowns. These devices use materials with lead equivalences of at least 0.25mm, which attenuates approximately 97% of the radiation at 70kVp. Devices with thicker lead equivalences will obviously be more effective at attenuating radiation of higher energy. A useful form of shielding is air. Air is a good absorber of radiation. Increasing the amount of air gap between you and the radiation source is equivalent to increasing distance. Increase the shielding, decrease the dose.
It is the responsibility of the radiographer to manage radiation dose, and all three of these strategies should be used to minimise dose to both staff and patients. Most of these strategies are applied automatically by a good radiographer.
Known as the "As Low As Reasonably Achievable," or ALARA, principle, this includes taking radiographs based on the patient's needs (as determined by an examination), using the fastest film compatible with the diagnostic task, collimating the beam to a size as close to that of the film as feasible and using leaded aprons and thyroid shields when they would not interfere with the image. Some radiographers prefer the time ALARP or "As Low as Reasonably Practicable" but the two terms are equivalent in meaning and purpose.
ALARA is an important requirement as there are no limits on dose to patients for medical purposes. The only requirement is that the dose must be justified on medical grounds.
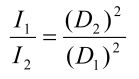
The Inverse square law is based on basic Newtonian physics and can be applied to gravitation of planets, electrostatic forces between electrically charged particles, acoustics and electromagnetic radiation. It is applicable to the radiographer as doubling the distance away from the x-ray source quarters the dose received. Conversely, halving the distance, increases the radiation level by a factor of four. Good use of inverse square law principles can yield significant reductions in both patient and operator radiation exposures.

Lead (Pb) gowns are generally provided in two thicknesses - 0.35mm Pb and 0.5mm Pb. As shown in the following table, 0.5mm of lead is sufficient to reduce the energy of a 200kVp xray beam by 50%. Since most medical xray machines have a maximum kVp of 140, this is more than sufficient protection!
Go Back to General Radiography Section
Radiation protection is an important consideration due to the potential for ionization radiation (x-rays) to disrupt the molecular structure of organic cells, which may result in functional impairment of tissues and organs. The potential damage is related to the exposure, the duration of exposure and the area of tissue exposed.
Time, Distance & Shielding
These are the three cardinal rules of dose reduction and radiation safety
Time - refers to the length of exposures, in that shorter exposures will produce less radiation dose. This can be controlled by reducing the mAs used in general radiographic practice and minimising the screening time in fluoroscopy. Halve the time, halve the dose.
Distance - refers to the distance between an individual and the radiation source (eg the X-ray tube). This is the most effective method of minimising dose to staff members, even small increases in distance can result in significant dose reductions. Double the distance, quarter the dose.
Shielding - refers to both fixed protective barriers and personal protective equipment, such as lead gowns. These devices use materials with lead equivalences of at least 0.25mm, which attenuates approximately 97% of the radiation at 70kVp. Devices with thicker lead equivalences will obviously be more effective at attenuating radiation of higher energy. A useful form of shielding is air. Air is a good absorber of radiation. Increasing the amount of air gap between you and the radiation source is equivalent to increasing distance. Increase the shielding, decrease the dose.
It is the responsibility of the radiographer to manage radiation dose, and all three of these strategies should be used to minimise dose to both staff and patients. Most of these strategies are applied automatically by a good radiographer.
ALARA - As low as Reasonably Achievable
ALARA is an important requirement as there are no limits on dose to patients for medical purposes. The only requirement is that the dose must be justified on medical grounds.
Inverse Square Law
The Inverse square law is based on basic Newtonian physics and can be applied to gravitation of planets, electrostatic forces between electrically charged particles, acoustics and electromagnetic radiation. It is applicable to the radiographer as doubling the distance away from the x-ray source quarters the dose received. Conversely, halving the distance, increases the radiation level by a factor of four. Good use of inverse square law principles can yield significant reductions in both patient and operator radiation exposures.
Radiation spreads out as it travels away from the X-ray source. Therefore, the intensity of the radiation follows Newton's Inverse Square Law. As shown in the image above, this law accounts for the fact that the intensity of radiation becomes weaker as it spreads out from the source since the same amout of radiation becomes spread over a larger area. The intensity is inversely proportional to the distance from the source. Basic dose intensity can be calculated using the following formula.
Lead Gowns

Radiographer wearing lead protective apparel
Lead (Pb) gowns are generally provided in two thicknesses - 0.35mm Pb and 0.5mm Pb. As shown in the following table, 0.5mm of lead is sufficient to reduce the energy of a 200kVp xray beam by 50%. Since most medical xray machines have a maximum kVp of 140, this is more than sufficient protection!
| Peak Voltage (kVp) | Half Value Layer (mm) |
| 50 | 0.06 |
| 100 | 0.27 |
| 150 | 0.30 |
| 200 | 0.52 |
| 250 | 0.88 |
| 300 | 1.47 |
| 400 | 2.5 |
| 1000 | 7.9 |
Go Back to General Radiography Section