Neonatal Abdominal Radiography
Introduction
'Cotside' abdominal radiography in the neonatal unit presents a number of radiographic challenges. This page considers the radiographic techniques required for particular pathologies and line placements.
Abbreviations and Terminology
UAC:
UVC:
ETT:
NGT:
TPT:
VP Shunt:
CVC:
VLBW:
NEC:Umbilical artery catheter
Umbilical vein catheter
Endotracheal tube
Nasogastric tube
Transpyloric tube
Ventriculo-peritoneal shunt
Central Venous Catheter
Very Low Birthweight
Necrotising Enterocolitis
Ground Rules
You learn quickly that radiography in the neonatal unit is different. The patients are very small, vulnerable and sometimes very ill. The following are some very simple dot point tips:
- wash your hands before entering the unit and on exiting. Also, wash your hands between babies (important)
- ensure that the baby's name matches the one on the request form (careful you don't get confused with twins)
- check the clinical information on the request form- this can influence what you include on the image
- don't run the mobile machine into the cot/incubator (surprisingly easy to do)
- ask the nurses for help- they know the babies, know their illnesses, and are used to handling them
- be careful to avoid patient rotation, particularly with chest radiography
- use a side marker (see Baker Cone)- left and right are not always clear from the anatomy, particularly in chest radiography
- check departmental protocol re removal of ECG leads
- think about radiation protection- horizontal ray technique considerations, gonad protection, long bone protection, the nurse's fingers
- you are not the boss- if the nurse says the baby can't be moved..the baby can't be moved.
- use a cassette tray if there is one built into the cot/isolette
Technique Tips
- I have noticed that some radiographers set an approximate neonatal exposure (kV, mAS) in advance i.e. before they leave for the unit, on the way, or on arrival at the unit. The reason for this is that the previous exposure might be an adult exposure. It is possible that in concentrating on the positioning task that you might overlook setting the exposure. This could be a disaster if the previous exposure was for an adult abdomen in ICU with a grid (I have seen it happen). This practice is not required if there is a dedicated mobile X-ray machine for the neonatal unit.
Radiation Protection
Operator Irradiation
Side Markers
Side markers in the neonatal unit are important. The difficulty is that your side marker can appear to be almost as big as the baby's chest. There are three solutions that I am aware of
Baker ConesDedicated Neonatal MarkersBaker cones are pieces of lead rubber that have the side marker punched into them.
The side marker on the left is simply too large for use in the Neonatal Unit. You don't want to collimate out to include this relatively large marker. The side marker on the left is the type used by the radiographers at the Adelaide Womens and Childrens Hospital. They also use these small side markers with the operator's initials. Importantly, the operator's initials are engraved laterally on the marker- to the right on a right marker and to the left on a left marker. This ensures that if the marker is partly collimated off, it is the operator's initials that are collimated off and not the "L" or "R".
Lead on Plastic MarkersThese markers work on the opposite principle to brass engraved markers. They are usually a lead letter stuck onto a plastic base material. The image from these markers is less bulky/conspicuous than that produced by a brass engraved side marker
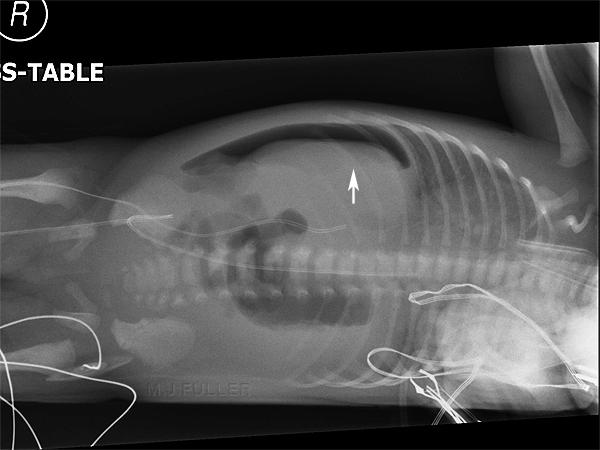
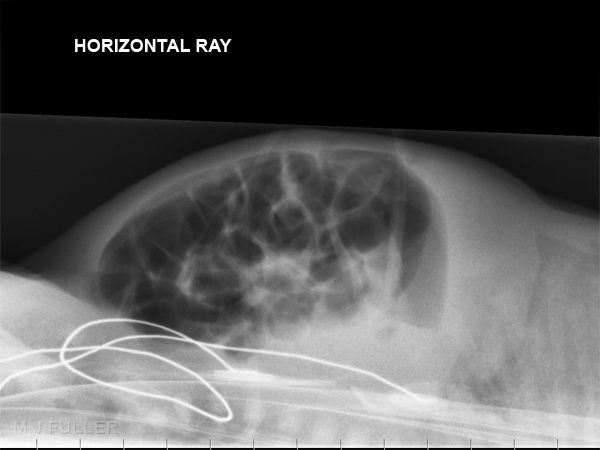
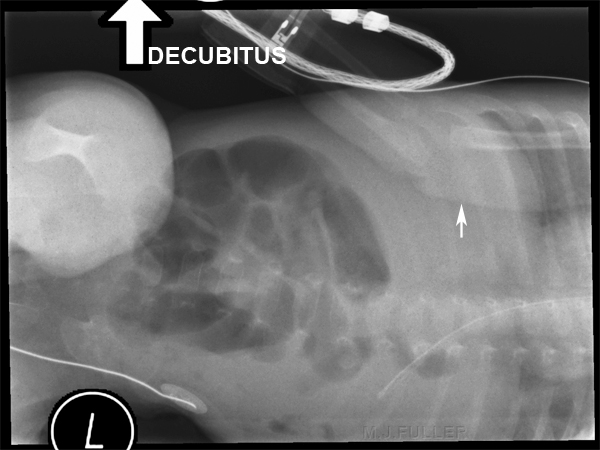
Left Lateral Decubitus
Right Lateral Decubitus
Supine Decubitus
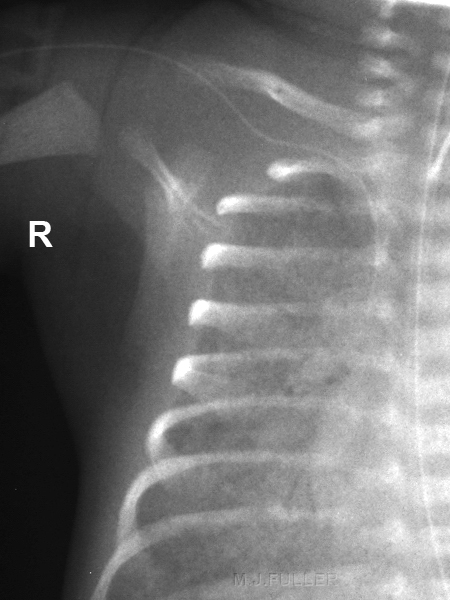
The baby's right arm is superimposed over the chest/abdomen (white arrow). This is highly undesirable when you are looking for free gas sited at the lateral aspect of the liver
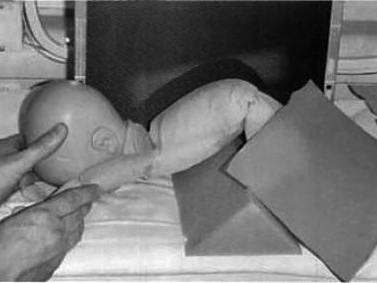
Imperforate Anus
There is a specific abdominal radiography technique for imperforate anus. The position and image are shown below.
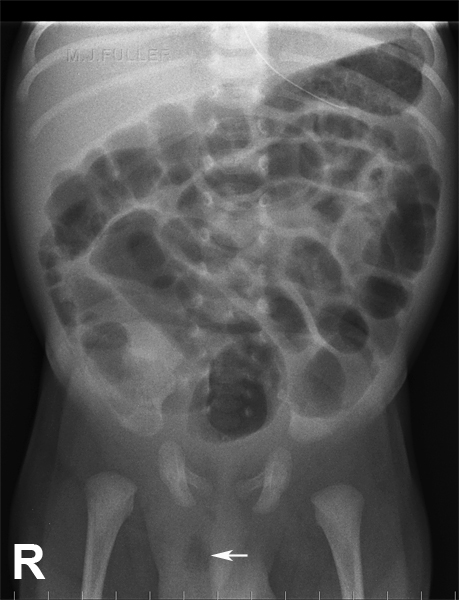
Inguinal Hernia
Inverted lateral rectum position
<a class="external" href="http://books.google.com.au/books?id=vgHF3KvGFzcC&pg=PA126&lpg=PA126&dq=neonatal+radiography&source=web&ots=j0frDYgDKU&sig=wpdDsFTjxLl5wtz0z3Eb5K-cydU&hl=en&sa=X&oi=book_result&resnum=6&ct=result#PPA125,M1" rel="nofollow" target="_blank">Source: Maryann Hardy and Stephen Boynes, Paediatric Radiography, 2003</a>Horizontal ray lateral rectum with lead shot marker
indicating the position of the anus
Source: Maryann Hardy and Stephen Boynes, Paediatric Radiography, 2003
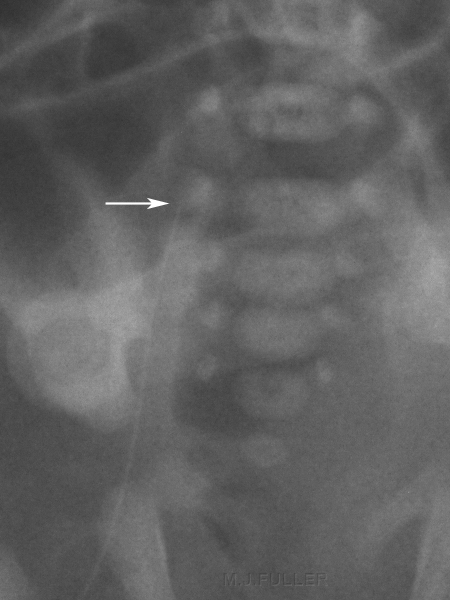
This baby has an inguinal hernia with air-filled bowel within the scrotum (bottom arrow)
The artifact is an umbilical clamp (top arrow)
Tubes, Lines and Catheters
You may be called to the Neonatal Unit to confirm the position of a line, tube or catheter. A knowledge of these lines will be useful in determining which anatomy should be included on the image (i.e. it will determine your beam coning).
Umbilical Catheters
UVC
- The umbilical vein is 2-3cm long and 4-5mm in diameter
- From the umbilicus, it passes cephalad and a little to the right. It joins the left branch of the portal vein after giving off several large intrahepatic branches.
- The ductus venosus arises from the point where the UV joins the left portal vein.
UAC
- The umbilical arteries are the direct continuation of the internal iliac arteries.
- A catheter passed into an umbilical artery will usually (but not always) enter the aorta via the internal iliac artery.
- Occasionally it will pass into the femoral artery via the external iliac artery or into the gluteal arteries.
- The femoral and gluteal arteries are unsuitable sites for sampling, infusion, or blood pressure monitoring.<a class="external" href="http://www.adhb.govt.nz/newborn/Guidelines/VascularCatheters/UmbilicalCatheters.htm#UAC" rel="nofollow" target="_blank">source</a>
There are two potential positions for the UAC. These are described as "high" or "low".
- The high position is at the level of thoracic vertebral bodies T6-T9. This position is above the coeliac axis (T12), the superior mesenteric artery (T12-L1), and the renal arteries (L1). This position is essentially "above the diaphragm".
- The low position is at the level of lumbar vertebral bodies L3-L4. This position is below the structures as above, and is above the aortic bifurcation (L4-L5). The inferior mesenteric artery arises from L3-L4. This position is essentially "above the bifurcation". <a class="external" href="http://www.adhb.govt.nz/newborn/Guidelines/VascularCatheters/UmbilicalCatheters.htm#UAC" rel="nofollow" target="_blank">source</a>
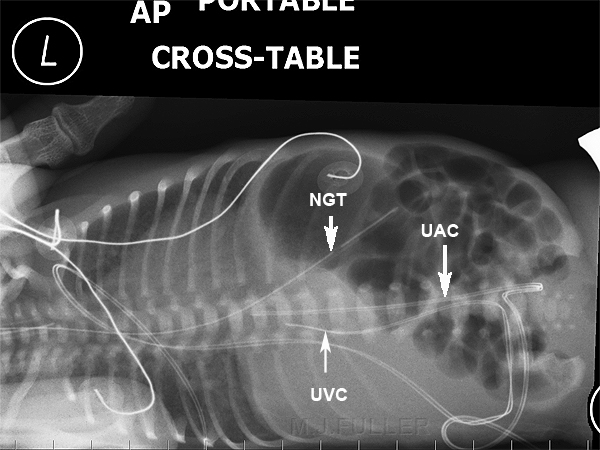
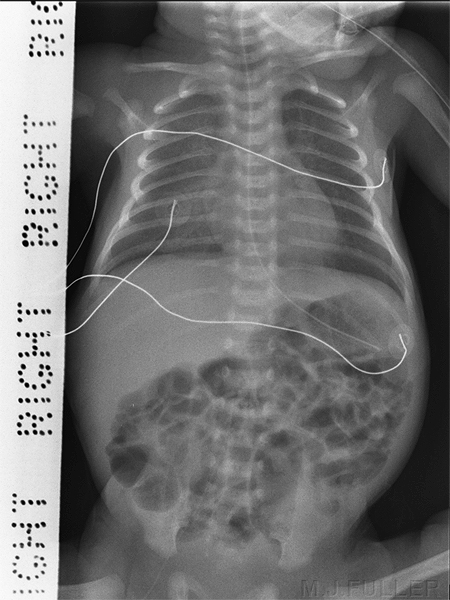
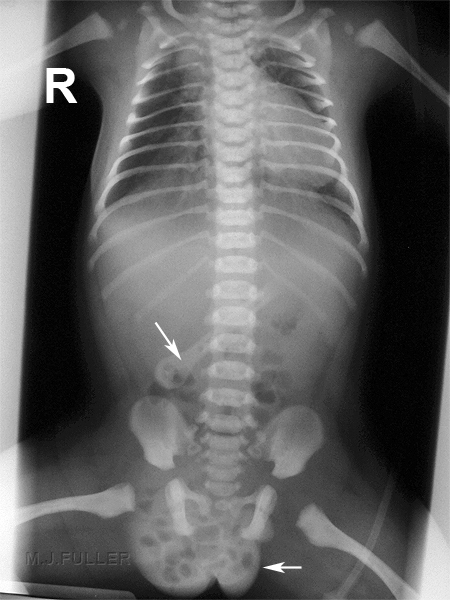
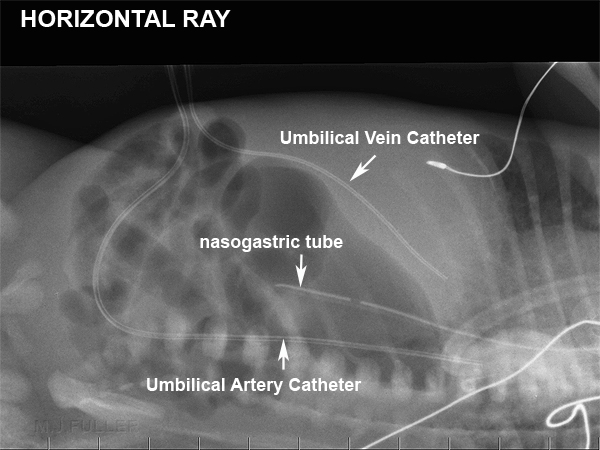
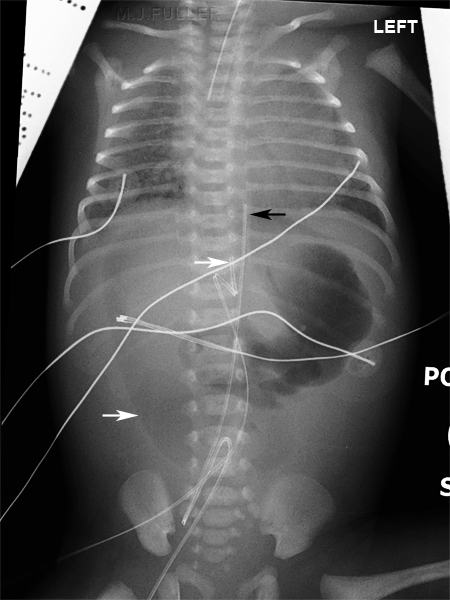
<img align="bottom" alt="Umbilical catheter position" height="600" src="http://image.wikifoundry.com/image/1/GWJuIjLId0OcSBW_Q3X4rg131678/GW450H600" title="Umbilical catheter position" width="450"/> The umbilical catheters are inserted through the umbilicus into either the umbilical vein or the umbilical artery. The umbilical artery catheter (UAC) characteristically deviates inferiorly before tracking up the aorta. See the lateral decubitus abdominal image below for further appreciation of the course of the umbilical artery.
The umbilical vein catheter takes a completely different course along the umbilical vein. See also below
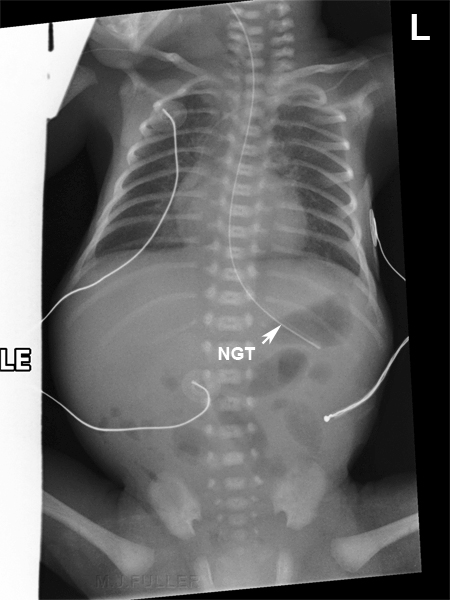
Double lumen catheters can be used in babies who are very sick and may require significant supportThe UAC and UVC are seen in this dorsal decubitus abdominal image.
UAC
The umbilical artery catheter (UAC) can be seen to track inferiorly and posteriorly from the umbilicus before tracking up the aorta.
UVC
The umbilical vein catheter(UVC) takes a shorter course along the umbilical vein.
NGT
The nasogastric tube enters the stomach from the oesophagus. When assessing the position of the NGT the position of the sidehole should also be considered.
Nasogastric Tube
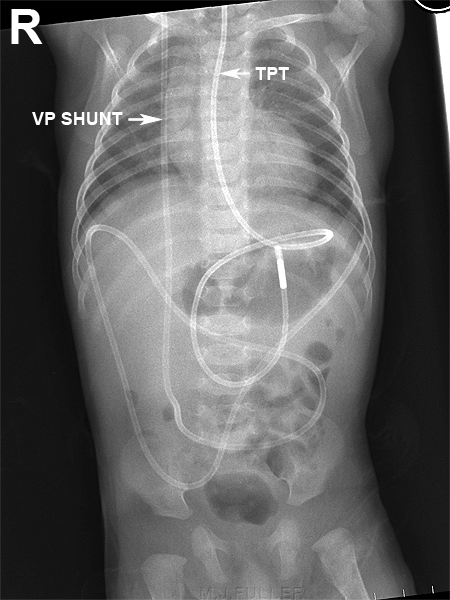
Transpyloric Tube and VP Shunt
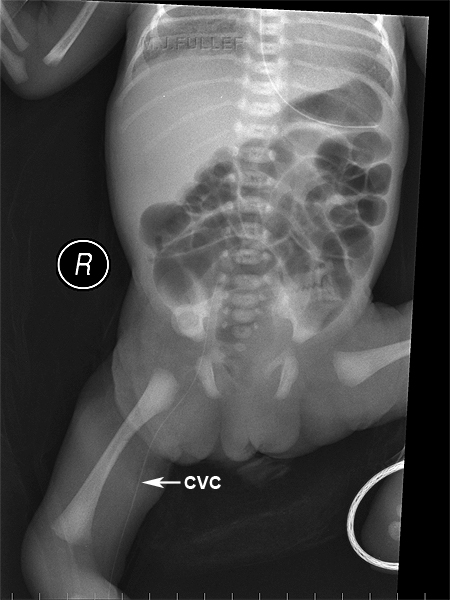
Central Venous Catheter (CVC) Longline- leg
The central venous catheter has been inserted in the right leg and its tip is difficult to localise precisely. This is a common problem with CVC lines and emphasises the need for good quality images when checking CVC lines. A study of printed CR images vs soft copy CR images reported a long line detection rate of 66.7% vs 95.6% respectively. <a class="external" href="http://www.pubmedcentral.nih.gov/picrender.fcgi?artid=1721656&blobtype=pdf" rel="nofollow" target="_blank">(A Evans, J Natarajan, C J Davies, 2004).</a>
Other suggestions include
"The authors emphasise the importance of verifying neonatal long line position using contrast, as the exact localisation of the catheter tip can be difficult on plain radiographs. As an alternative, Groves et al have described the use of colour Doppler to aid ultrasonographic line tip visualisation." <a class="external" href="http://fn.bmj.com/cgi/content/extract/91/4/F311" rel="nofollow" target="_blank">T M Berger, M Stocker, J Caduff</a>
Gonad protection could have been used to good effectA magnified view demonstrates the CVC tip to be at the level of the first sacral vertebra. This is an "actual pixels" image i.e. one pixel in the image is one pixel on the screen. This demonstrates the advantage of viewing images by 'softcopy' rather than hardcopy
Central Venous Catheter (PICC) - arm
The technique issues are much the same as for a leg longline. Include the arm of interest and a good exposure is required. A softcopy digital image is best.
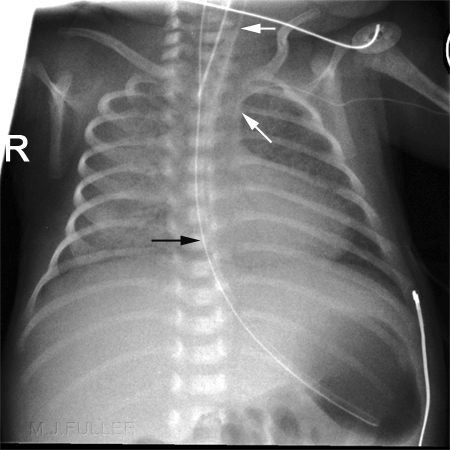
The tip of the longline is in the proximal brachiocephalic vein. (lower white arrow)
The top white arrow identifies the endotracheal tube (ETT)
The black arrow identifies the nasogastric tube (NGT)
Case Study
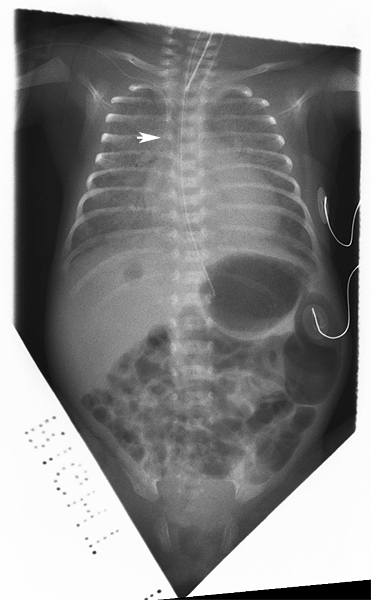
The radiographer was called to the Neonatal Unit and requested to undertake a chest/abdominal X-ray examination on one of the premature babies to establish the position of the double lumen Umbilical Vein Catheter (UVC). The image is shown below
Discussion
This page covers a range of radiographic techniques, interventions and pathologies that you might encounter in a neonatal unit. An awareness of this material will make a trip to the neonatal unit more meaningful and possibly more effective.
...back to the Applied Radiography home page