Ingested/Aspirated Foreign Body Radiography
If you are a radiographer employed in an acute care facility, radiography for identification and localisation of ingested/aspirated foreign bodies will present a familiar scenario. This page considers radiographic techniques for visualisation of ingested/aspirated foreign bodies.
Ingested Foreign Body
Ingested or Inhaled?
Children have a natural tendency to put things in their mouths- and those things are not always food! I have received referrals for foreign body radiography where the referring doctor has not made it clear whether he/she thinks the patient has inhaled or ingested the foreign body. It is essential that you ask the parents/carer what they know about the ingestion/aspiration of the foreign body. Sometimes there is a clear history of witnessed foreign body ingestion/aspiration. At the other end of the scale, I have seen a child present for possible ingestion of a foreign body based entirely on a history of the parents not being able to find the batteries for the television remote control!
A commonly seen dilemma is encountered with radiography of children in cases where it is not clear whether the patient has aspirated or inhaled a foreign body (or neither). Should you be imaging the thorax, abdomen or both? This may end up a judgement call, but relevant considerations should include the following
- what was the history and what are the clinical signs?
- should the child be subject to radiographic imaging at all if the ingested foreign body is considered benign/low risk?
- the child will receive a much lower radiation dose with chest radiography than abdominal radiography
- the upper airway should be included in the imaging if aspiration is being investigated
- the chest radiography and abdominal radiography should overlap images
- If the foreign body is known to be metallic (or relatively radiopaque) can you safely halve the mAS?
- if you have a sample of the foreign body, should it be imaged separately?
- should a single exposure of the chest and abdomen be attempted, or should separate exposures be made for chest and abdomen?
Ingested Blunt Objects
American Society For Gastrointestinal Endoscopy
Guideline for the management of ingested foreign bodies,
GASTROINTESTINAL ENDOSCOPY VOLUME 55, NO. 7, 2002</a>Ingestion of blunt foreign bodies does not usually present a great risk to the adult patient unless the foreign body is greater in diameter than 2.5cm and/or is lodged in the patient's oesophagus and/or is composed of a toxic material.
With larger objects, good clinical management may require serial radiographs. This may appear a tedious exercise to the radiographer, but may be justified where there is a risk of complications. A low radiation exposure technique may be considered, but such a technique may impede diagnosis of subtle pneumoperitoneum (Riglers sign)'.
Two radiographic views at 90 degrees (AP and lateral) will assist in identifying the exact location of a foreign body (although this is not commonly performed).
Case 1
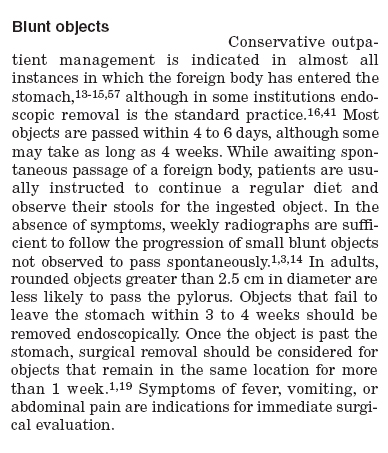
<a class="external" href="http://kara.allthingsd.com/files/2008/05/thousand_marble3.jpg" rel="nofollow" target="_blank">http://kara.allthingsd.com/files/2008/05/thousand_marble3.jpg</a>This 9 year old patient presented to the Emergency Department with a history of ingested glass marble. This is likely to be an accurate history given that the patient is 9 years old and able to provide an accurate history of accidental ingestion. The marble is made of glass and used by children in a <a class="external" href="http://www.landofmarbles.com/marbles-play.html" rel="nofollow" target="_blank">game</a>. The parents sensibly brought a marble with them to the Emergency Department. The radiographer imaged the marble first. Whilst it could be argued that the glass marble would be expected to be demonstrated on the plain film, it was a low cost exercise and provided additional diagnostic confidence. The referring doctor asked for a single exposure of the chest and abdomen which the radiographer has attempted to provide. The marble is clearly evident and is probably located in the pyloris. Given the clear history of ingestion, a collimated abdominal image may have been more appropriate. Consideration should be given to the level of distress experienced by the patient. If the foreign body is lodged in the oesophagus, the patient will be likely to be experiencing considerable distress and may be producing abnormal amounts of saliva. (if you drink a carbonated drink- i.e. soda, pop, softdrink- you may experience an acute dilation of the oesophagus which is sufficiently painful to bring a tear to the eye!)
Ingested Long Objects
Long objects such as cutlery will have difficulty passing through the sweep of the deuodenum and are usually removed surgically.
Ingested Sharp Objects
American Society For Gastrointestinal Endoscopy
Guideline for the management of ingested foreign bodies,
GASTROINTESTINAL ENDOSCOPY VOLUME 55, NO. 7, 2002</a>Patients with ingested sharp-pointed objects are more likely to be subject to daily abdominal radiography. A low-dose technique would be prudent in patients with dense radiopaque foreign bodies. A thin object such as a razor blade can be difficult to visualise if it happens to be overlying the patient's spine at the time of imaging. Pneumoperitoneum may be missed if a low-dose technique is employed (radiographer judgement call).
Inhaled Foreign Body
Inspiration and Expiration Technique
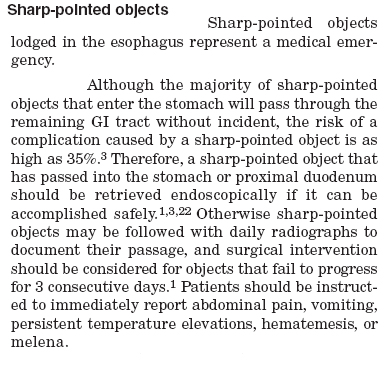
Inspiration and expiration PA/AP chest radiography is a commonly employed series for inhaled foreign body radiography in children. If an inhaled foreign body is present, it can produce a one-way or ball-valve effect. This may over-expand the lung distal to the foreign body. The over-expanded lung will tend to remain a constant volume on inspiration, expiration and decubitus views/techniques.
Dr Helen Williams noted the following in respect of inhaled foreign bodies. "An inhaled foreign body (FB) in a child can be easily missed if the diagnosis is not considered, particularly if a history of choking or coughing is not forthcoming, or the episode of aspiration is unwitnessed. Once the diagnosis is suspected a chest radiograph (CXR) is invariably requested. This may provide clues to the diagnosis but a normal CXR does not rule out FB aspiration. Radio-opaque foreign bodies are easily localised, usually within a major airway. However, it can be difficult to identify the radiographic signs associated with an inhaled FB that is not radio-opaque—for example, food or small plastic objects. The presence of an intraluminal FB within the trachea or a bronchus often results in secondary changes in the associated lung or pulmonary lobe. One of the most important signs to identify is obstructive emphysema, or overinflation of the lung or lobe distal to the airway obstruction"
<a class="external" href="http://ep.bmjjournals.com/cgi/content/extract/90/2/ep31" rel="nofollow" target="_blank">Dr Helen Williams
ILLUMINATIONS </a><a class="external" href="http://ep.bmjjournals.com/cgi/content/extract/90/2/ep31" rel="nofollow" target="_blank"> Inhaled foreign bodies </a>
<a class="external" href="http://ep.bmjjournals.com/cgi/content/extract/90/2/ep31" rel="nofollow" target="_blank">http://ep.bmjjournals.com/cgi/content/extract/90/2/ep31</a>
Decubitus Technique
Jayesh M Bhatt, VikkiAnn Lee, Penny Broadley commented on Dr Helen Williams article as follows "Williams [1] highlights the key points in the management of inhaled foreign bodies (FB). One of the important points is to request inspiratory and expiratory chest radiographs if FB aspiration is suspected. Because young children are unable to co-operate, paired inspiratory and expiratory films are not always possible. The lateral decubitus film is a useful and convenient method to determine the presence of air trapping [2] a... When the child is placed on his side, the splinting of the dependent hemithorax results in restriction of movement of the thoracic cage on that side and under aeration of the lung while the hemithorax on the opposite side is unrestricted and the lung is well aerated"
<a class="external" href="http://ep.bmj.com/cgi/eletters/90/2/ep31#44" rel="nofollow" target="_blank">Jayesh M Bhatt, VikkiAnn Lee, Penny Broadley</a><a class="external" href="http://ep.bmj.com/cgi/eletters/90/2/ep31#44" rel="nofollow" target="_blank">
The lateral decubitus film to determine the presence of air trapping
http://ep.bmj.com/cgi/eletters/90/2/ep31#44
BMJ. 2 August 2005</a>
Case 1
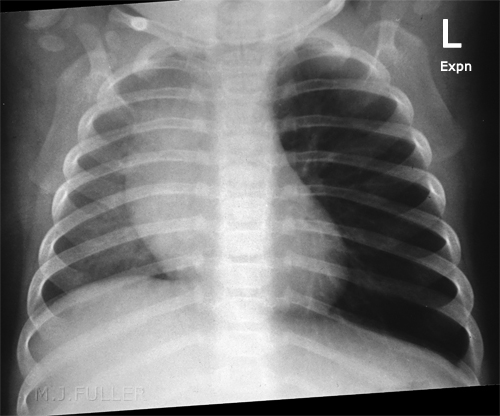
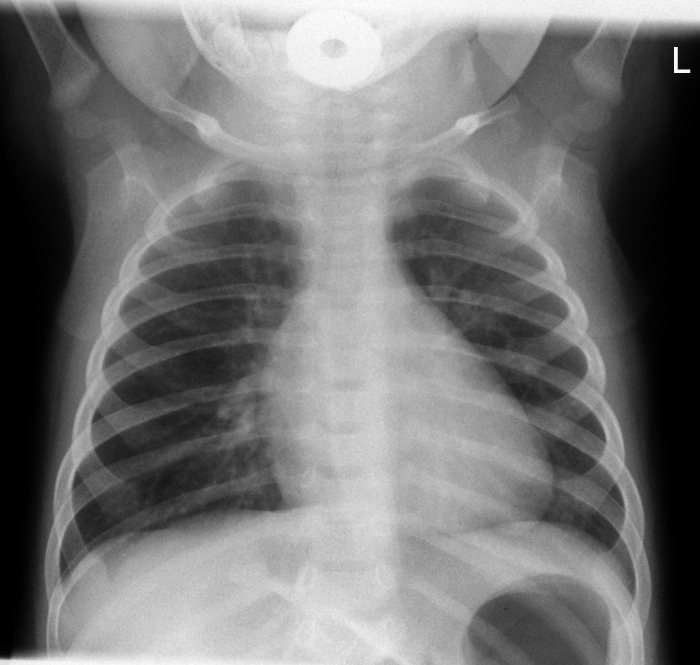
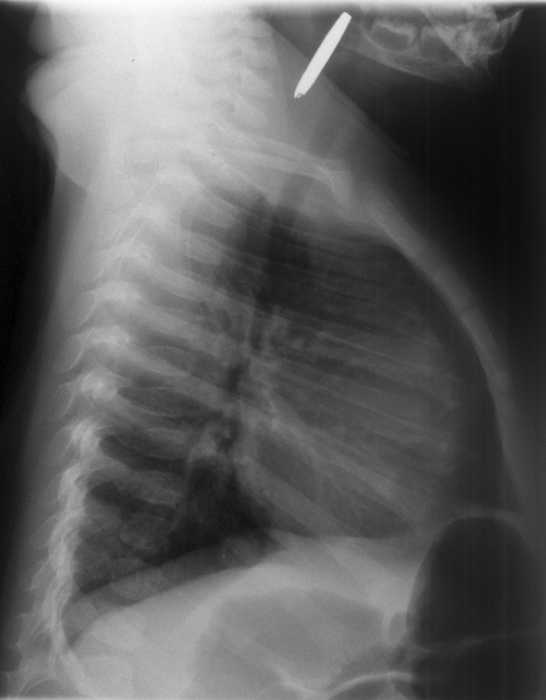
This 7 month old boy presented to the Emergency Department after a choking episode. There was concern about an inhaled foreign body. Inspiration and expiration chest radiography was requested.
Case 2
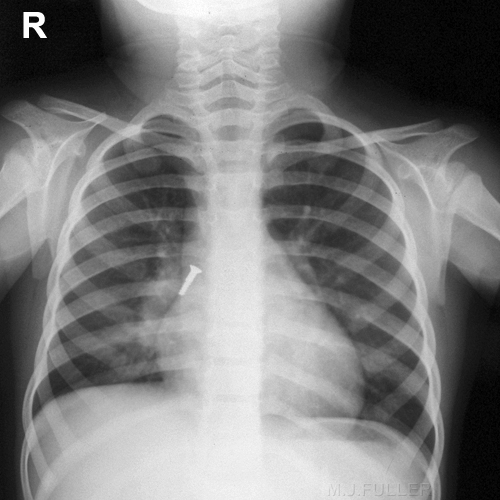
This case is circa 1958. The details of the case are unknown.
There is a bolt in the right main bronchus The bolt appears to have moved distally into a RLL bronchus.
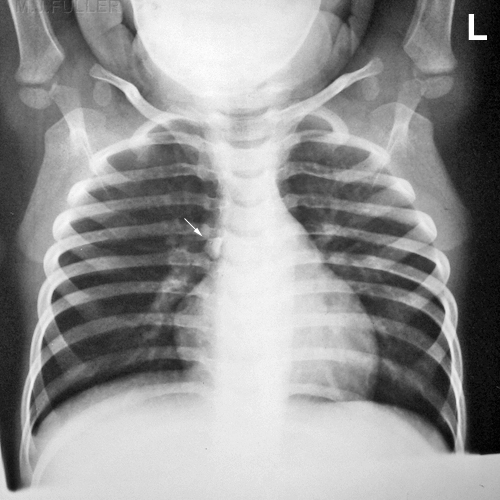
Case 3The details of the case are unknown.
There is a piece of gravel in the right main bronchus.(arrowed)
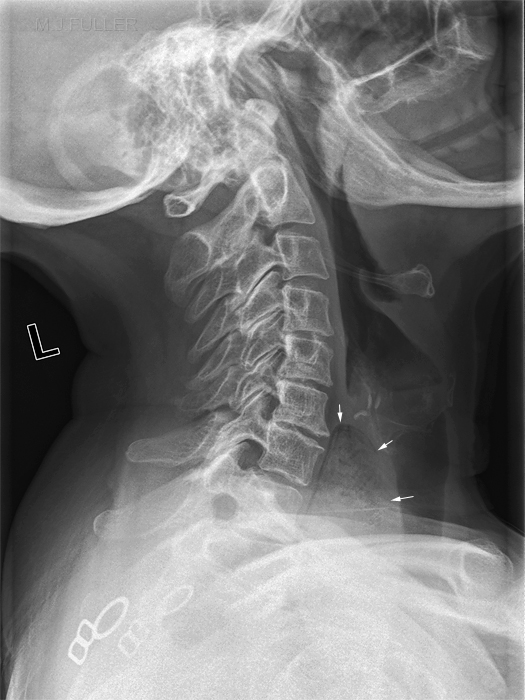
Lateral Soft Tissue Neck for Foreign Body
Foreign Body TrackingLateral soft tissue neck radiography is similar to lateral cervical spine radiography. It should be remembered that the cervical spine is posterior to the airway/GIT soft tissues and that a lateral soft tissue neck view should include oropharynx soft tissues.
Case 1
Case 2
Case 3
Case 4
Case 5
Case 1
The Unexpected Foreign Body
... back to the Wikiradiography Home page
... back to the Applied Radiography home page