Exposure Index
Jump to navigation
Jump to search
| Exposure index (EI) is the measure of the amount of exposure received by the image receptor (IR). It is dependent on mAs, total detector area irradiated, and beam attenuation. The exposure index is indicative of the image quality. Equipment manufacturers provide a recommended EI range for optimal image quality (Bontrager & Lampignano, 2005, p. 52). The Internet allows you to access information from anywhere, and at any time. However, the knowledge you retrieve may be a confusing collection of information in a wide variety of formats. Online information, along with your print resources, must ALWAYS be evaluated for relevance, currency, reliability, accuracy and coverage. For example, I read on a website that Adolf Hitler escaped Germany at the end of the war in a U-boat and traveled to a German base in Antarctica. Another website claims that DR has greater spatial resolution and uses less radiation dose than CR Both these claims are ridiculous, yet one of them keeps turning up in a CSU Wagga prac report ( and it does not involve a U-boat!) EI in digital radiography can be compared to film speed and blackening in film-screen. When film was used, the accuracy of the exposure was obvious based on the appearance of the image. Digital systems post-process images and display adequate contrast and brightness at a much wider range. Therefore, adequate exposure can only be assessed through image noise or burn-out. Secondary workstations such as those used by technologists for image review, are often of lower resolution and brightness than those used for diagnosis. Because of this, it is often difficult to assess whether an image is noisy or not. The exposure index is meant to be an indication of whether the noise levels are acceptable (AAPM, 2009). Errors in the calculation can occur resulting in an inaccurate EI. This can arise when the software fails in determining which part of the image is the patient anatomy, for example, in the presence of gonadal shielding or prosthesis. EI cannot be solely relied on, therefore the technologist must remain critical of the appearance of the image and the accuracy of the EI (AAPM, 2009). EI is derived from the mean detector entrance exposure which is derived from the mean pixel value of the image. Most systems use a histogram analysis in order to calculate the mean pixel value (Neitzel, 2004, p. S231). 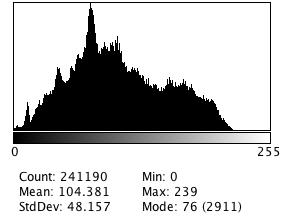 This is a histogram created from an AP pelvis radiograph. The x-axis represents the pixel value while the y-axis represents the number of pixels with that value. The mean pixel value here is 104.381. Although EI is always derived from the IR exposure, equipment manufacturers calculate the numeric value differently, resulting in different ranges and definitions (Carlton & Adler, 2006, p. 367; Neitzel, 2004, p. S231). Also, there is variation between units purchased from the same manufacturer based on different IRs and software (Carlton & Adler, 2006, p. 367). Different IRs have different detective quantum efficiency (DQE). A high DQE results in lower noise levels (AAPM, 2009, p. 3). Therefore, all systems have a different index and are difficult to compare across systems. Fuji CR Fuji uses a sensitivity number (S) that is related to the amount of amplification required by the photomultiplier tube to adjust the digital image. S is inversely proportional to exposure. Properly exposed images should have an S between 150-250 (Carlton & Adler, 2006, p. 367). Kodak CR Kodak uses the term Exposure Index, which is directly proportional to exposure. Properly exposed images should have an EI between 1,800-2,200 (Carlton & Adler, 2006, p. 367). A change of 300 in the EI indicates a change of a factor of 2 in the exposure to the IR. Agfa CR Agfa uses log median exposure (LgM). This system compares the exposure level of the image to a baseline established for the department. Since it is based on a log system, an increase of 0.3 means the dose was doubled (Carlton & Adler, 2006, p. 367). An optimal exposure lies between 1.9 and 2.5. Philips DR Philips uses an EI that is inversely proportional to exposure. This index is represented in bigger discrete steps (eg., 100, 125, 160, 200, 250, 320, 400, 500, etc). Each step requires a 25% change in exposure to occur (AAPM, 2009). An optimal exposure lies between 200 and 800. Imaging Dynamics DR Imaging Dynamics uses f#. The f# compares the exposure to an established target exposure. Negative values represent underexposure, while positive values indicate overexposure (AAPM, 2009). Canon DR Canon uses a reached exposure value (REX). REX is a function of the brightness and contrast as selected by the operator (AAPM, 2009). GE DR GE uses the detector exposure index (DEI) which compares the detector exposure to the expected exposure value (AAPM, 2009). Siemens Siemens uses an Exposure Index (EXI). EXI is calculated by dividing the field into a 3x3 matrix and assessing only the central segment, and is based on the selected organ program. EXI is directly proportional to dose. Doubling dose doubles the EXI. EXI depends on organ program, whether manual exposure or AEC was used, and the measuring field (AAPM, 2009). Future Developments In 2008, the International Electrotechnical Commission (IEC) developed and published the International Standard IEC 62494-1 on the definition and scaling of the exposure index for digital radiography. According to the standard the EI shall be proportional to the exposure (air kerma) and shall be scaled as EI = 100 * X, where X is the air kerma at the detector, at the calibration beam quality. It is expected that this standard definition will be implemented in future digital radiography systems. The American Association of Physicists in Medicine (2009), published a document in July, 2009 with the purpose of identifying a standard index which reflects the adequacy of the exposure received by the IR. References American Association of Physicists in Medicine. (2009). An Exposure Indicator for Digital Radiography. Retrieved from http://www.aapm.org/pubs/reports/rpt_116.pdf Bontrager, K. L., & Lampignano, J. P. (2005). Textbook of radiographic positioning and related anatomy (6th ed.). Elsevier Science. Carlton, R. R. & Adler, A. M. (2005). Principles of radiographic imaging: An art and a science. Delmar Learning. International Electrotechnical Commission (2008). IEC 62494-1 ed. 1 Medical electrical equipment - Exposure index of digital x-ray imaging systems - Part 1: Definitions and requirements for general radiography Neitzel, U. (2004). Management of pediatric radiation dose using Philips digital radiography. Pediatric Radiology, 34(Suppl 3), S227-S233. |