Cervical Myelography
Jump to navigation
Jump to search
Introduction
Anatomy
Preparation
Tray Setup
Radiographic Technique
Imaging
Limitations of Myelography
Technique Tips
Complications
After Care
...back to the Applied Radiography home page
Introduction
IndicationsA cervical myelogram is the radiographic demonstration of the cervical spinal cord following the injection of a contrast media agent into the cerebrospinal fluid within the subarachnoid space.
- neck and arm pain and weakness
- most commonly performed today on patients who are unable to have MRI assessment of their spinal cord
- non-consent by patient to procedure
- contrast or iodine allergy
- pregnancy (pregnancy test compulsory for women of child-bearing age in some centres)
- bleeding disorders, blood thinning medications , anticoagulants (heparin, warfarin, aspirin etc)[ check I.N.R. if available]
- arachnoiditis
- abnormal ICP
- blood in CSF
Anatomy
<a class="external" href="http://www.frca.co.uk/article.aspx?articleid=100126" rel="nofollow" target="_blank">http://www.frca.co.uk/article.aspx?articleid=100126</a>
<a class="external" href="http://www.health.com/health/library/mdp/0,,zm2346,00.html" rel="nofollow" target="_blank">
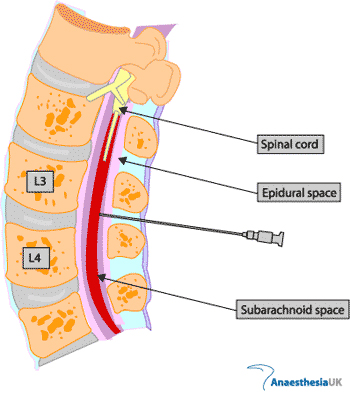
</a>The spinal cord is not imaged directly in myelography- rather, it is the subarachnoid space that is covering the spinal cord that receives the contrast media and is therefore imaged.
The contrast media can be injected directly into the subarachnoid space at the cervical level, however, this is not the preferred method and is a rarely used technique. The preferred technique is to inject the contrast media into the subarachnoid space and 'flow' it up to the cervical region.
Preparation
- patient identification (3 Cs- correct patient, correct side, correct procedure)
- Patient should be wearing a hospital gown; pants, socks and shoes removed
- consent form
- Fast from solids for 4 - 6 hours prior to procedure
- collect relevant previous imaging for ease of access prior to procedure
- A premed' of 10mgs of oral valium will reduce patient anxiety levels
- injection site shaved as deemed necessary
- advise the CT scanning radiographer when you are about to start the procedure (patient will be sent to CT for a CT myelogram after the procedure)
- patient should empty his/her bladder prior to the procedure
- ensure lab form is completed
Tray Setup
10 - 12 mls contrast medium ( non-ionic contrast) 1 anti-septic skin prep solution 1 vial local anaesthetic 1 sterile gloves 3 basins 1 band-aid 1 pack towels 1 pack gauze sponges 1 fenestrated drape 1 10ml glass syringe for contrast 1 10 ml plastic syringe for local anaesthetic 1 drawing up cannula 1 18g 38mm needle for local anaesthetic 1 23g 32mm needle for injecting local anaesthetic 1 22g 90mm spinal needle 1 extension tubing 1 one-tap stopcock plastic tap
Radiographic Technique
Preparation
- Cervical myelography is best performed as a fluoroscopy procedure using a C-arm unit
- contrast media is commonly injected at the level of lumbar L2/3 or L3/4
- Contrast media can be injected directly into the subarachnoid space at the cervical level if required
- obtain consent and explain procedure to patient
- cervical preliminary/scout images should be taken (AP, lateral, swimmers)
- for a lumbar injection, the patient is positioned prone on the fluoroscopy table with a pillow or sponge under his/her abdomen to reduce the lumbar lordosis
Direct Cervical Injection
- Position the patient prone on the fluoroscopy table with his/her feet on the footplate. A sponge under the patients feet will improve patient comfort
- fluoroscopy table horizontal
- The patient's neck is extended and placed on a foam block. The patient should be asked at this stage whether they will be able to tolerate this position for the length of the procedure (at least 1/2 hour)
- The patient's arms should be immobilised at his/her sides with straps and the patient should have handgrips positioned at a comfortable level.
- rotate the C-arm into the cross-table lateral position and centre to the C1/C2 level- ensure the patient's cervical spine is perfectly lateral.
- a pair of forceps and a black felt-tip pen will be used by the radiologist to mark a spot on the skin for needle placement. This point will be between the first and second cervical vertebra spinous processes and at the level of the lower AP 1/3rd.
- the radiologist will apply a skin prep and the patient will have a drape covering applied.
- the radiologist will inject local anaesthetic at the needle entry site.
- The radiologist will insert the 22 gauge spinal needle into the subarachnoid space and manipulate the needle until cerebrospinal fluid (CSF) is seen to drip from the needle when the stylet is removed. Keep the needle horizontal- never angle anteriorly. CSF is collected for laboratory analysis
- 8 - 10 mls of contrast media is injected into the subarachnoid space. Select a larger field of view such that the patient's clivis is visualised. Screen while the contrast is injected to ensure that it remains within the cervical lordosis.
- tilt the table as required to keep the contrast media in the cervical lordosis. Care must be taken at all times to ensure that the contrast media does not spill past the foramen magnum into the ventricles
- the spinal needle is removed by the radiologist ready for imaging
Lumbar Injection
- for a lumbar injection, the patient is positioned prone on the fluoroscopy table with a pillow or sponge under his/her abdomen to reduce the lumbar lordosis
- raise the head of the table 30 - 45 degrees
- select and mark the level of puncture (L2/3 or L3/4)
- The radiologist will clean the skin and drape
- local anaesthetic will be injected to anaesthetise the needle insertion site
- The spinal needle is inserted midline angles in a cephalic direction to 'pass under' the spinous process. The spinal needle can be inserted obliquely if there are 'kissing' spinous processes
- screen intermittently to assess the position of the spinal needle
- collect CSF- 10 drops per specimen container x 3. Specimen containers should be numbered to reflect the order in which specimens were taken
- inject contrast agent under fluoroscopic control.
Imaging
- The radiographer must ensure that the contrast bolus remains within the cervical region during imaging. All of the contrast can be lost to the cranial subarachnoid space very quickly if sufficient care is not taken.
- Imaging is as follows
- lateral with traction on patient's arms
- AP
- Coned AP of foramen magnum
- 30 and 55 degree obliques
- Swimmers lateral with C1 included in image
- AP and obliques of cervico thoracic junction is required
- All images should have a landmark reference- either C1 or the first rib
- The patient should have CT myelogram imaging within 2 - 3 hours
Imaging
AP Scout/Prelim Swimmers Scout/prelim Lateral Scout/Prelim Lateral 30 degree Oblique 55 degree oblique AP coned Cranio-cervical junction 30 degree Oblique 55 degree Oblique Swimmers
Limitations of Myelography
"The most important limitation of myelography is its inability to visualize entrapment of the nerve root lateral to the termination of the nerve root sheath. It is thus unable to detect any far lateral disc herniations." (AMERICAN FAMILY PHYSICIAN, JUNE 1, 2002 / VOLUME 65, NUMBER 11 www.aafp.org/afp p 2303
Technique Tips
- imaging must occur immediately after contrast injection because contrast is absorbed quickly
- The contrast will flow 'downhill' very quickly if the patient is rolled into the lateral decubitus position- beware and screen frequently to monitor movement of the contrast column.
- It is highly desirable to have two radiographers undertaking a cervical myelogram- one can operate the C-arm and the other can help move the patient when required
Complications
- dural tear
- headache
- infection
- Nerve root damage
- Meningitis
- Epidural abscess
- Contrast reaction (anaphylactic shock)
- CSF leak
- Haemorrhage
- nausea and vomiting
After Care
- rest and increased fluid intake will help to reduce headaches post myelogram
- Monitoring required
- Head and shoulders elevated 30 to 45 degrees
- Bed rest for several hours
- Puncture site checked before release
...back to the Applied Radiography home page