CT Case 1 - Iatrogenic Venous Air Embolism
Jump to navigation
Jump to search
Introduction
A CTPA was performed on a 45 year old male who presented with central chest pain and a past history of PE and DVT.
Results
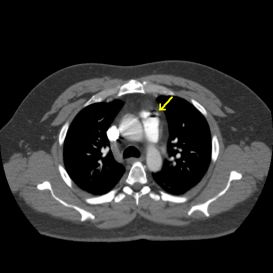
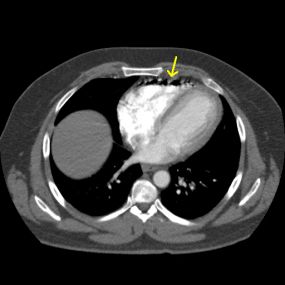
No PE detected. Multiple small locules of gas visualised in the main pulmonary artery (Image A) and the right ventricle (Image B) consistent with iatrogenic venous air emboli.
CT Appearance
Venous air emboli appear as hypodense (black) bubbles of air at the most anterior aspects of hyperdense (white) contrast filled vessels and heart chambers.
Discussion
Iatrogenic venous air emboli (VAE) are visualised on a CT scan when air is inadvertently injected into the venous system during intravenous (IV) contrast administration. Small VAEs (a few millilitres of air with visualised air bubbles less than 10mm in diameter) occur in approximately 11-23% of CT scans performed with IV contrast and are usually asymptomatic. VAEs are classed as being medium sized if several small bubbles or a 1-2cm diameter bubble is visualised on the subsequent CT scan. Massive VAEs (>200ml of air) are considered to be fatal however there are reports of fatalities from 100mls of air and there are reports of people surviving after 135ml of air has been inadvertently injected instead of contrast media during a CT scan using a contrast pump.
During a contrast enhanced CT scan air can be inadvertently introduced into the venous system at a number of stages including the initial insertion of the IV cannula, flushing of the cannula with saline, from air within the connecting tube, air within the injector syringe, or as a result of microbubbles within the contrast media itself. The air enters the venous system due to the pressure gradient between the site of entry and the right atrium.
Small and medium VAEs are usually asymptomatic but signs and symptoms of larger ones are non-specific and may include:
Small to medium VAEs usually do not require any treatment other then close observation and documentation of the occurance. The treatment for larger VAEs is to place the patient in the Durant position which is the left lateral decubitus position with the head down 30-45˚ (Trendelenberg position). This position allows the air bubbles to rise to the apex of the right ventricle and prevent them from entering the pulmonary vascular system or blocking the outflow from the right heart causing an “air-lock” and leading to circulatory failure. Also, 100% oxygen should be administered to increase oxygenation as this is believed to help nitrogen gas to be reabsorbed from the air bubbles and reduce their size. In severe cases hyperbaric oxygen therapy is required.
Conclusion
Iatrogenic VAE is a potentially fatal side effect of contrast enhanced CT. Small volumes of air usually do not cause any side effects but accidental injection of large volumes of air can be fatal. VAE is preventable and should not occur if particular care and attention is given when the contrast is drawn up, and when priming connecting tubes, connecting to the IV cannula and during prelimary flushing of the IV cannula. Two people (nurse/radiographer and consenting doctor) should routinely check the syringe and connecting tube for significant volumes of air and the presence of multiple air bubbles before contrast injection is commenced.
References
Husain, S, Ahmed, L, & Al-Sawwaf, M (2006) ‘Venous air embolism from intravenous CT contrast administration’, Journal of the American College of Surgeons, Vol. 202, No. 1, p 197.
Imai, S, Tamada, T, Gyoten, M, Yamashita, T, & Kajihara, Y (2004) ‘Iatrogenic venous air embolism caused by CT injector – from a risk management point of view’ Radiation Medicine, Vol. 22, No. 4, pp 269-271.
Pham, K & Cohen, A (2003) ‘Iatrogenic venous air embolism during contrast enhanced computed tomography: a report of two cases’, Emergency Radiology, Vol. 10, pp 147-151.
Introduction
A CTPA was performed on a 45 year old male who presented with central chest pain and a past history of PE and DVT.
Results
No PE detected. Multiple small locules of gas visualised in the main pulmonary artery (Image A) and the right ventricle (Image B) consistent with iatrogenic venous air emboli.
Image A Iatrogenic venous air embolism visualised in the main pulmonary artery as small locules of gas.
Image B Multiple small locules of gas within the right ventricle consistent with iatrogenic venous air emboli.
CT Appearance
Venous air emboli appear as hypodense (black) bubbles of air at the most anterior aspects of hyperdense (white) contrast filled vessels and heart chambers.
Discussion
Iatrogenic venous air emboli (VAE) are visualised on a CT scan when air is inadvertently injected into the venous system during intravenous (IV) contrast administration. Small VAEs (a few millilitres of air with visualised air bubbles less than 10mm in diameter) occur in approximately 11-23% of CT scans performed with IV contrast and are usually asymptomatic. VAEs are classed as being medium sized if several small bubbles or a 1-2cm diameter bubble is visualised on the subsequent CT scan. Massive VAEs (>200ml of air) are considered to be fatal however there are reports of fatalities from 100mls of air and there are reports of people surviving after 135ml of air has been inadvertently injected instead of contrast media during a CT scan using a contrast pump.
During a contrast enhanced CT scan air can be inadvertently introduced into the venous system at a number of stages including the initial insertion of the IV cannula, flushing of the cannula with saline, from air within the connecting tube, air within the injector syringe, or as a result of microbubbles within the contrast media itself. The air enters the venous system due to the pressure gradient between the site of entry and the right atrium.
Small and medium VAEs are usually asymptomatic but signs and symptoms of larger ones are non-specific and may include:
- acute shortness of breath ± coughing
- chest pain
- cyanosis
- hypotension
- pulmonary oedema
- paralysis
- seizures
Small to medium VAEs usually do not require any treatment other then close observation and documentation of the occurance. The treatment for larger VAEs is to place the patient in the Durant position which is the left lateral decubitus position with the head down 30-45˚ (Trendelenberg position). This position allows the air bubbles to rise to the apex of the right ventricle and prevent them from entering the pulmonary vascular system or blocking the outflow from the right heart causing an “air-lock” and leading to circulatory failure. Also, 100% oxygen should be administered to increase oxygenation as this is believed to help nitrogen gas to be reabsorbed from the air bubbles and reduce their size. In severe cases hyperbaric oxygen therapy is required.
Conclusion
Iatrogenic VAE is a potentially fatal side effect of contrast enhanced CT. Small volumes of air usually do not cause any side effects but accidental injection of large volumes of air can be fatal. VAE is preventable and should not occur if particular care and attention is given when the contrast is drawn up, and when priming connecting tubes, connecting to the IV cannula and during prelimary flushing of the IV cannula. Two people (nurse/radiographer and consenting doctor) should routinely check the syringe and connecting tube for significant volumes of air and the presence of multiple air bubbles before contrast injection is commenced.
References
Husain, S, Ahmed, L, & Al-Sawwaf, M (2006) ‘Venous air embolism from intravenous CT contrast administration’, Journal of the American College of Surgeons, Vol. 202, No. 1, p 197.
Imai, S, Tamada, T, Gyoten, M, Yamashita, T, & Kajihara, Y (2004) ‘Iatrogenic venous air embolism caused by CT injector – from a risk management point of view’ Radiation Medicine, Vol. 22, No. 4, pp 269-271.
Pham, K & Cohen, A (2003) ‘Iatrogenic venous air embolism during contrast enhanced computed tomography: a report of two cases’, Emergency Radiology, Vol. 10, pp 147-151.