Ultrasound Physics
Jump to navigation
Jump to search
Definition of Ultrasound
ultrasound is sound with frequency greater than 20,000 cycles per second or 20kHz. Audible sound sensed by the human ear are in the range of 20Hz to 20kHz.
Advantages
Ultrasound can be directed as a beam.
Ultrasound obeys the laws of reflection and refraction.
Ultrasound is reflected by objects of small size.
Disadvantages
Ultrasound propagates poorly through a gaseous medium.
The amount of ultrasound reflected depends on the acoustic mismatch.
Creating an ultrasound image is done in three steps - producing a sound wave, receiving echoes, and interpreting those echoes.
Producing a sound wave
- Ultrasound waves are produced by a transducer. A transducer is a device that takes power from one source and converts the energy into another form eg electricity into sound waves. The sound waves begin with the mechanical movement (oscillations) of a crystal that has been excited by electrical pulses, this is called the piezoelectric effect.
-

- The sound waves are emitted from the crystal similar to sound waves being emitted from a loud speaker. The frequencies emitted are in the range of (2- 15MHz) and are unable to be heard by the human ear. Several crystals are arranged together to form a transducer. It is from the transducer that sound waves propagate through tissue to be reflected and returned as echoes back to the transducer.
- Sound is produced using Piezoelectricity which is the ability of some materials (notably crystals and certain ceramics) to generate an electric charge in response to applied mechanical stress, the reverse applies when
- The word is derived from the piezoelectric effect is reversible in that materials exhibiting the direct piezoelectric effectconverse piezoelectric effect (the production of stress and/or crystals will exhibit a maximum shape change of about 0.1% of the original dimension.
- Precise electrical pulses from the ultrasound machine make the transducer create sound waves at the desired frequency. The sound is focused either by the shape of the transducer (Curved, Linear, Sector) or a set of control pulses from the ultrasound machine. This focusing produces the desired shaped sound wave from the face of the transducer. The wave travels into the body and comes into focus at a desired depth.
- On the face of the transducer a rubber material enables the sound to be transmitted efficiently into the body. This rubber coating is required for impedance matching and allows good energy transfer from transducer to patient a vice versa. To help with the transmission of sound waves a water based gel is placed between the patient's skin and the probe.The gel establishes good acoustic contact with the body, since air is a very good acoustic reflector.
Receiving the echoes
- The image is formed by the reverse of the process used to create the sound waves. The returning echoes to the transducer are converted by the crystals into electrical signals and are then processed to form the image.
Forming the image
- To form the image ultrasound machine needs to determine the direction of the echo, how strong the echo was and how long it took the echo to be received from when the sound was transmitted. Once the ultrasound scanner determines these three things, it can locate which pixel in the image to light up and to what intensity. (direction and the travel time give the location, how strong gives the intensity)
Sound in the body
- When a sound wave encounters a material with a different density (acoustic impedance), part of the sound wave is reflected back to the transducer and is detected as an echo. The time it takes for the echo to travel back to the transducer is measured and used to calculate the depth of the tissue interface causing the echo. The greater the difference between acoustic impedances, the larger the echo is. (larger reflection)
- Highly reflective interfaces give rise to a strong echo which is represented on the screen as a bright spot, whilst the opposite is true of weak reflective interfaces. Areas without acoustic interfaces such as the lumen of vessels and other cavities containing liquid (blood, bile, ascites or urine) give no reflection and no spot on the screen ie a black space on the monitor. If the waves hits gases or solids the density difference is so great that most of the acoustic energy is reflected and it becomes impossible to see deeper.
- The speed of sound is different in different materials, and is dependent on the acoustical impedance of the material. However, the ultrasound scanner assumes that the acoustic velocity is constant at 1540 m/s. An effect of this assumption is that in a real body with non-uniform tissues, the beam becomes de-focused and image resolution is reduced.
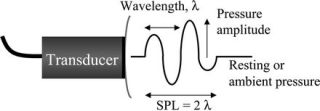
- The formula for the velocity of sound is (velocity = frequency x wavelength). The frequencies used for medical imaging are generally in the range of 2 to 15 MHz. Higher frequencies have a smaller wavelength (as can be seen from the formula for velocity of sound), and can be used to make images with smaller details. However, the attenuation of the sound wave is increased at higher frequencies, so in order to have better penetration of deeper tissues, a lower frequency 3-5 MHz is used. Seeing deep structures in the body with ultrasound is very difficult as some acoustic energy is lost every time an echo is formed, but most of it is lost from acoustic absorption.
Apparatus
Scanner types
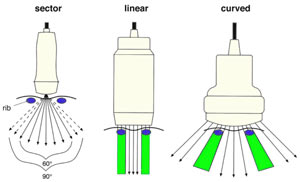
For abdominal ultrasound curved type scanners are used as the best compromise of two other standard type probes the linear and the sector scanner.
Linear - the linear array scanners produce sound waves parrallel to each other and produces a rectangular image. The width of the image and number of scan lines are the same at all tissue levels. This has the advantage of good near field resolution. Often used with high frequencies ie 7MHz. Can be used for viewing surface texture of the liver. There disadvantage is artifacts when applied to a curved part of the body creating air gaps between skin and transducer.
Sector/Vector - Produces a fan like image that is narrow near the transducer and increase in width with deeper penetration. It is useful when scanning between the ribs as it fits in the intercostal space. The disadvantge is poor near field resolution. (why? the beam is diverged, so no focus?)
Curved - Often with frequencies of 2 - 5 MHz (to allow for a range of patients from obese to slender). It is a compromise of the Linear and Sector scanners. The density of the scan lines decreases with increasing distance from the transducer. Can be difficult to use in curved regions of the body eg. the spleen behind the left costal margin.
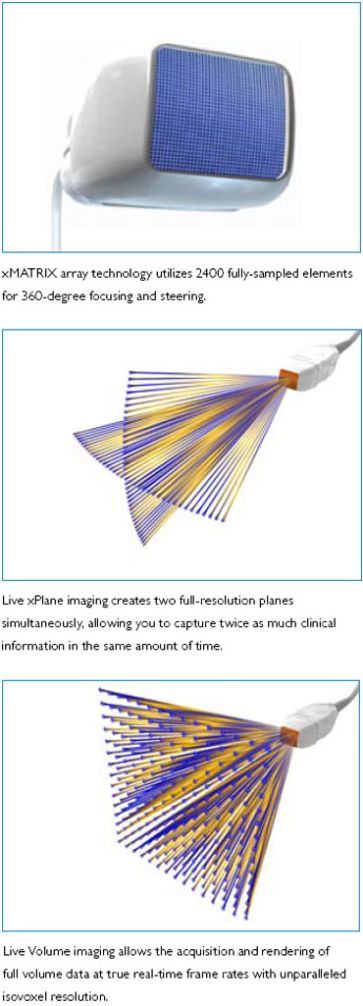
3D Transducers
Matrix Transducer- 3 to 1 MHz extended operating frequency range
- 2D Matrix phased array with 2,400 elements
- 2D, biplane (Live xPlane), triggered full volume, Live 3D Echo, Color Doppler with 2D, biplane and 3D,Harmonic Imaging
Mechanical 3D Tranducer
- 6 to 2 MHz extended operating frequency range
- Supports high resolution 2D imaging
- high resolution, quantitative, single sweep 3D volume aquisition
- 4D imaging up to 36 volumes per second
- Color Doppler
- Field of view: 66 degrees
- General purpose abdominal, obstetricaland gynecological applications

Controls

Ultrasound machines have a large array of options and features. The basic controls that you need to familiarize yourself in the early stages of learning are
Trackball - used for moving objects on the monitor (similar to using a mouse on the PC), it is used in conjunction with measuring, annotating, moving Res/Dopler boxes to the desired location. It has kidney buttons either side which are used to select functions (the same as clicking buttons on a mouse for the PC).
Freeze - This allows the image to be held (frozen) on the screen. While the image is frozen measurements can then be taken and organ annotations can be applied to the image before saving it.
Res or Zoom - This will allow magnification of areas of the ultrasound picture. Looking at Res/Zoomed areas of interest has the advantage of a more detailed view with the drawback of less anatomy visible to guide your movements.
Caliper - This is used to measure a distance (eg kidney length). It is used by selecting a starting spot by pressing a kidney key and using the trackball to measure to a second mark. The distance between the two marks will then be displayed on screen measured in cm. This can be used with other functions such as Res/Freeze.
Gain - This function is very similar to a brightness control. The echo signal returning to the body is converted into an electronic signal by the transducer. This electronic signal has to be amplified to produce images on the monitor. This signal amplification is called Gain and will regulate the strength of the echo’s being received.
Time Gain - Is an adjustment for the sensitivity at each depth to allow compensation for signal loss from deeper in the tissue. This can be set so that organs such as the liver will have uniform brightness at all depths. It is a series of multiple sliders so you can set the time gain differently for each depth.
BMode imaging Controls
Depth/F.O.V. Control- Varying the depth of the F.O.V. varies the write zoom and therefore the number of pixels per cm and spatial resolution potential of the system. It is important not to use excessively large F.O.V’s that reduce spatial resolution achievable but also not to ‘clip’ the F.O.V. too tightly around the region of interest such that relationships with other structures are not shown.
Gain- Refers to the degree of amplification applied to all returning signals. If set too low there will be underwriting of the image and real echo will be lost from the display. If set too high there will be overwriting of the display with artefactual noise introduced and also a reduction in contrast resolution as all echoes get progressively brighter.
T.G.C.- The T.G.C. control compensates for the effects of attenuation by progressively increasing the amount of amplification applied to signals with depth (time). The sonographer aims to produce an image of uniform brightness from top to bottom and this requires regular adjustment of this control during scanning.
Power or Output Control- This controls the strength of the voltage spike applied to the crystal at pulse emission. Increasing power output increases the intensity of the beam and therefore the strength of echo return to the transducer. i.e. increases signal to noise ration (SNR). However it also increases the patients ultrasound dose. It is best practice to operate on minimum power and maximum gain, remembering though that no amount of gain can compensate for insufficient power. The obvious alternative to increasing power output if ‘dropout’ artefact is encountered at depth is to use a lower frequency transducer.
Dynamic Range- Refers to the range of echoes processed and displayed by the system, from strongest to weakest. The strongest echoes received are those from the ‘main bang’ and transducer-skin interface and they will always be of similar strength. As DR is reduced therefore it is the echoes at the weaker end of the spectrum that will be lost. DR can be considered as a variable threshold of writing for weaker signals. For general imaging the DR should be kept at its maximum level to maximise contrast resolution potential. However in situations where low-level noise or artefacts degrade image quality the DR can be reduced to partially eliminate these appearances.
Focal Zones- Throughout the scan the sonographer should constantly check the position of the focal zone(s) and ensure they are at the depth of interest. Multiple focal zones can be used to maximise lateral resolution over depth if motion is not encountered, but it is important to minimise the focal zones used when assessing moving structures i.e. a fetal heart.
Artefacts
Reverberation is the persistence of sound in a particular space after the original sound is removed
How to Select the best transducer
Transducer selection is based on all the six F’s
-Frequency
-Format/F.O.V
-Footprint
-Frame Rate
-Focal Characteristic
-Functional Aspects
Frequency- It is best to use the maximum frequency possible to image the region of interest, allowing for adequate penetration to this depth and thus avoiding ‘dropout’ artefact. There are several reasons for this, increasing frequency will; improve axial resolution, produce a better beam shape (longer near field) and increase the return from non-specular interfaces. Transducer frequencies common today are 5-15MHz for superficial work and 2-7MHz for deeper areas.
Format- The depth of interest also influences the decision on transducer format used. Linear arrays with their rectangular field of view ( F.O.V.) provide the widest superficial F.O.V and best spatial resolution in the superficial zone. However when imaging to depth a transducer with a radiating scan format is needed to give a useful width to the F.O.V with depth. i.e. Convex, Phased and Annular arrays all have this radiating scan format. Convex arrays are the most common today.
Footprint- This refers to the area of the transducer face that contacts the patient. Footprint becomes significant when access is limited (i.e. between ribs or through cranial fontanelle). In these situations phased and annular arrays provide the smallest footprint. In contrast the wide footprint linear and convex arrays provide superior superficial imaging but can be more difficult to keep in complete contact with the skin.
Frame Rate- This refers to how many times a second the image is updated. The frame rate determines the temporal resolution potential of the system and therefore is important when assessing moving interfaces. Cardiac ultrasound is a classic example of a situation where frame rate is very important. Mechanical transducers are generally unsuitable for this work because their frame rates are too slow. Multiple focal zones are unheard of and the line densities used are much lower that for general imaging.
Focal Characteristics- Most systems now allow a variable depth of focus by varying the firing delays of the crystal elements across the array. It is important to keep the focal zone(s) to the depth of interest.
Functional Aspects- Will you need to perform colour or PW doppler during the examination and does the transducer have this capability. Not all transducers allow biopsy guides to be attached and specialised transducers need to the used for intracavity exams.