Toxic Megacolon
DefinitionAn understanding of toxic megacolon is important for radiographers because the diagnosis can sometimes be expedited by the radiographer and the condition is potentially life-threatening if treatment is delayed. Importantly, the radiographer should be aware of the need to critically examine the supine abdominal film for evidence of abnormal large bowel (dilated, oedematous, effaced), intramural gas, hepatic portal-venous gas and pneumoperitoneum. Consideration should be given to performing supplementary views where there is evidence of critical pathology (e.g. erect CXR for pneumoperitoneum). Inpatients with fulminant colitis may be referred for abdominal plain film every day- this is usually justified. When considering which order should be applied for ward patients waiting for plain film radiography, call for the ? toxic megacolon patient first.
Importance of Clinical ContextToxic megacolon is the clinical term for an acute toxic colitis with dilatation of the colon <a class="external" href="http://emedicine.medscape.com/article/181054-overview" rel="nofollow" target="_blank">(Deepika Devuni, http://emedicine.medscape.com/article/181054-overview)</a>. Radiographers can be confused by this condition- it is not a disease in itself- it is (commonly) a sign of fulminant inflammatory bowel disease.
A patient with life-threatening toxic megacolon will usually have obvious clinical signs- they are usually very sick! "A typical clinical presentation is the rapid onset of abdominal pain and diarrhoea, accompanied by a high fever and severe debilitation." Stephen R Baker, The Abdominal Plain Film, Appleton and Lange, 1990, p203
Value of the Plain Film
Stephen R. Baker in his book 'The Abdominal Plain Film' makes the following observation on the value of the plain film in patients with toxic megacolon
There are but very few life-threatening conditions in which the abdominal roetgenogram still remains the sole imaging study required to render an unequivocal diagnosis. Along with pneumoperitoneum, mesenteric ischaemia, small bowel obstruction, colonic volvulus, and emphysematous cholecystitis, toxic megacolon must be included on this short list. In most instances, the plain film appearance is so distinctive that no other diagnosis need be considered. Furthermore, because the barium enema is a dangerous examination in fulminant colitis, exposing the patient to a heightened risk of large bowel perforation, the crucial role of non-contrast abdominal radiographs cannot be overemphasized.Stephen R Baker
The Abdominal PLain Film
Appleton and Lange, 1990, p203
Serial Plain Films
If toxic megacolon is clinically suspected, patients are usually followed up with plain abdominal radiography every 12-24 hours, depending on the patient’s clinical condition. <a class="external" href="http://www.radpod.org/2007/07/05/toxic-megacolon/" rel="nofollow" target="_blank">(http://www.radpod.org/2007/07/05/toxic-megacolon/)
</a>
Plain Film AppearancesThe daily abdominal plain film on patients with fulminant colitis can be erroneously interpreted by radiographers as wasteful and an unneccesary radiation hazard for the patient.
- Dilation of the transverse colon/splenic flexure (greater than 6cm diameter).
- Alteration of normal wall contour (effacement, thumbprinting, pseudopolyps)
- Intraluminal gas
- Hepatic portal-venous gas
- Pneumoperitoneum
Thumbprinting
Bowel Wall Effacement
Psudopolyps
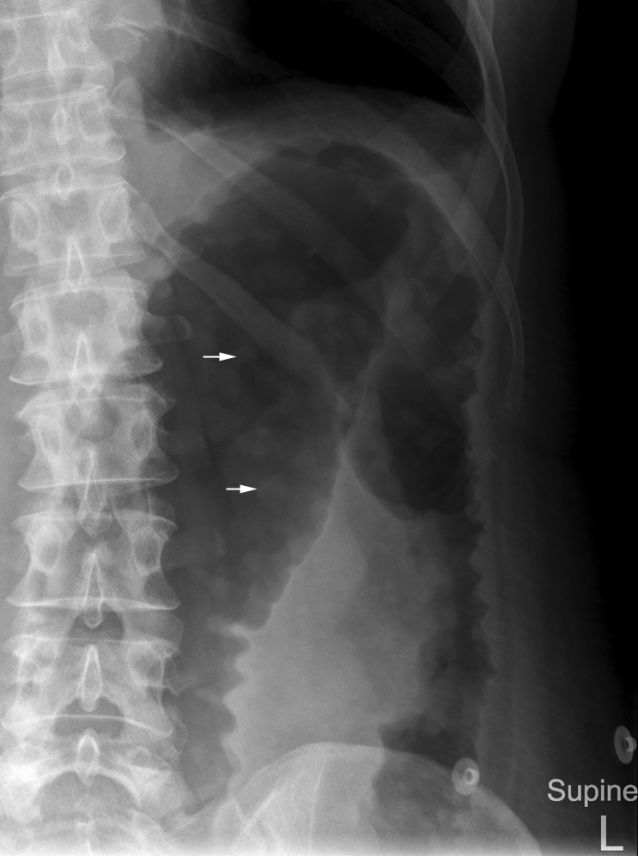
Pseudopolyps (white arrows) represent mucosal islands in denuded ulcerated colonic wall <a class="external" href="http://www.radpod.org/2007/07/05/toxic-megacolon/" rel="nofollow" target="_blank">(http://www.radpod.org/2007/07/05/toxic-megacolon/)
</a>
Intramural Gas
Pneumoperitoneum
Hepatic portal-venous gas
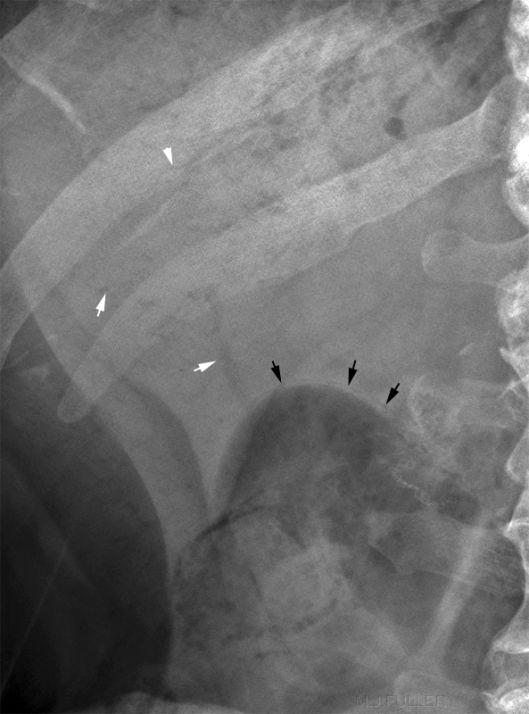
<img align="bottom" alt="portal venous gas" src="http://image.wikifoundry.com/image/1/jGWwjd2Ap2NdY6Fd58WtVA240521" title="portal venous gas"/> This is a magnified view of the erect abdominal plain film RUQ. The portal venous gas is clearly seen as well as intramural gas (black arrow) and surgical sutures (white arrow) in a patient with fulminant inflammatory bowel disease.
Notes
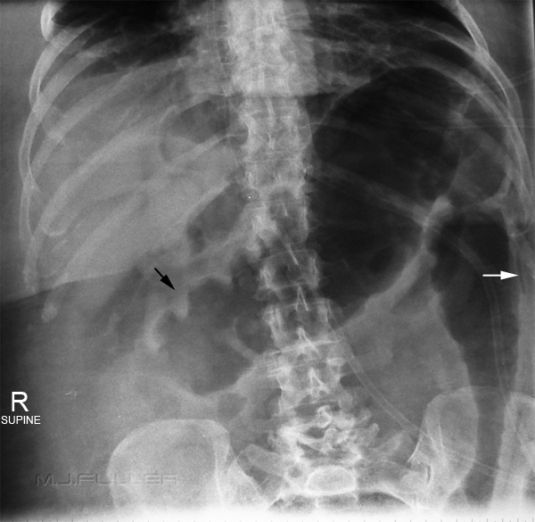
Case 11. Patients with toxic megacolon may demonstrate a remarkable similarity in the appearance of the large bowel on abdominal plain film. In particular, the mid-to-distal transverse colon only may appear to be involved. You should be mindful that this may be due to the highlighting of some of the diseased colon by the presence of intra-luminal gas. When the patient is supine, the transverse colon/splenic flexure are the least dependent segments of the large bowel- i.e. gas will tend to collect in the uppermost part of the bowel. If you can't see the remainder of the large bowel, how do you know whether it is similarly diseased? A prone abdominal film may reveal the diseased segments of large bowel to extend beyond that demonstrated in the supine image. Decubitus projections (left and right) will usually demonstrate involvement of both ascending and descending colon. The presence of toxic megacolon is more important than the extent- supplementary abdominal views should only be performed where their are sufficient indications.
2. Toxic megacolon is not well named. It is undeniably potentially toxic to the patient but it is not that 'mega'. When you compare the typical large bowel dilation that can occur with sigmoid volvulus (and some pseudo-obstructions), it might be more apt to have named it mild rather than mega.