Top 20 Practical Tips for Radiography in the Operating Theatre
Jump to navigation
Jump to search
Introduction
The operating theatre (OT) can be a confronting new environment for student radiographers. The best strategy for dealing with this problem is to take every possible opportunity to practise your operating theatre techniques. To help you along the way, here are 20 tips that you may find useful. Not all of these tips will be applicable to all theatre situations.
Tip 1. Get to Know Your Operating Theatre Staff
This is placed at number one for good reason. You are in their turf and you may have goals that conflict with theirs. For example, your goal to produce the best possible images may conflict with the scrub nurse's goal of keeping a sterile field intact!
Look at this theatre team..... they look like a team. You would be confident as a patient in their hands. This is how you should view your role in the operating theatre. You are joining a team of skilled people in the interest of a good surgical outcome for the patient.
These people can make your theatre experience very pleasant or very difficult. Engendering yourself to them can involve such things as
- learning their names
- learning their roles
- learning their rules.
- helping with patient transfers
Be a good communicator with the theatre staff
Tip 2. Know The Operating Theatre Rules
There's a good chance that the operating theatre will have several folders of protocols. These could cover aspects of theatre procedures such as attire, infection control, Occupational Health and Safety, patient safety etc. You will probably not be expected to study these protocols, but the few that affect you will need to be known.
Apart from the written rules, there are the matters of theatre culture. These are the rules that are not written down, but the staff tend to follow them- they are common understandings. It could cover such matters as how rules are followed, how they are policed, and how you get around them when required.
Tip 3. Assume Everything and Everyone is Sterile
Once the surgeon breaks the patient's skin, the patient is at risk of acquiring infection. One of the goals of the operating theatre staff is to prevent the patient developing a significant post-op infection.
You should be seen to be sharing in this goal. This will mean that you should take care not to touch anything or anyone that is sterile. This will mean not standing too close to a staff member who is gowned and gloved. It will also require you to point out to others in the operating theatre when they are at risk of breaching a sterile field, or indeed, when they have breached a sterile field.
Be particularly careful when you push the image intensifier over a patient- ensure that you do not touch the sterile handle attached to the operating light.
Tip 4. Know Your Image Intensifier
I am assuming that the majority of the imaging procedures in the operating theatre utilise the image intensifier. This machine's operation you will need to be understood very well. Modern digital image intensifiers have a number of pre and post-processing features. It is very embarrassing if you don't know how to perform a task on the image intensifier. This is particularly so when the surgeon knows that other radiographers have performed the task.
A surgeon will probably forgive you for not being familiar with a surgical procedure, but will be less forgiving if you are struggling to use the image intensifier.
If you are unfamiliar with a procedure, there can be much to be said for introducing yourself to the surgeon and advising him/her that you know how to use the image intensifier, but will need guidance with the procedure. Questions like..."which side would you like me to come in from?"or"do you want the image intensifier to go under the table or over the table for the lateral"
Good communication will suggest to the surgeon that you deserve his/her confidence in your abilities.
Tip 5. Know Your Procedures
There will be a variety of procedures that you will be expected to assist with. The surgeon will look to you for signs of confident and competent operation of the equipment. This will be very difficult if you are unfamiliar with a procedure.
If you are unfamiliar with a procedure, let the surgeon know. Better to let the surgeon know up front, than for the surgeon to find out during the procedure.
Also, if you know you have never seen a procedure that you have been called to do, ask another radiographer to come with you to help explain what is happening.
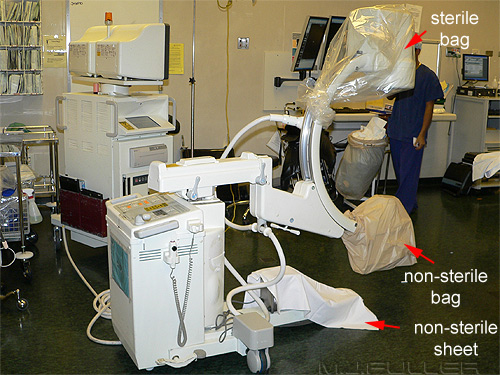
Tip 6. Cover/Drape Your Image Intensifier
Tip 7. Face the Monitor Cart Panel Towards Where you are Standing
It is better to spend 5 minutes at the beginning of an operation covering your image intensifier than to spend 20 minutes at the end of an operation cleaning off blood and betadine.
Set up the monitor cart so that the control panel is facing you. If you need to manipulate the image, you do not want to be wasting time walking around the cart. This will not apply to all image intensifiers.
Tip 8. Identify Your Patient
This might seem self-evident, but can be remarkably difficult in reality. You can't ask the patient what their name is. The most common method for identifying then patient is from the name on the paperwork in the theatre. Bear in mind that sometimes patient notes are swapped or there may be patient notes in theatre left from a previous patient.
Beware....
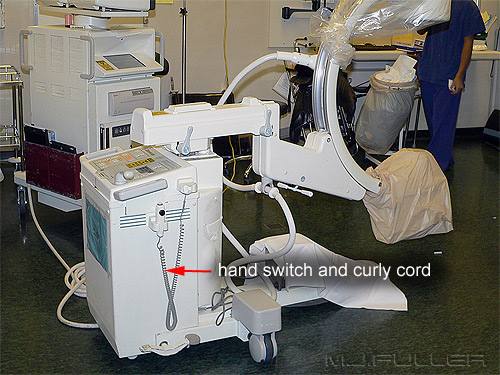
Tip 9. Secure your Plug
10. Go to the Toilet Before you Start
Securing the mains cord to the boom with a self tightening knot has two advantages.
Firstly, if someone trips over the cord, they will not rip the cord out of its socket (they may break their neck, but you’re machine is OK!). If the plug is pulled out of the socket, it could cause damage to your image intensifier, or you could lose images. Also, the surgical procedure will be delayed while you re-boot the image intensifier.
Secondly, when there are multiple sockets with multiple plugs, you will recognize your plug immediately.... it’s the one with the fancy knot (I have pulled out the patient’s ventilator plug by mistake). Any knot that tightens as you pull on it would be suitable.
Many image intensifiers have a built in uninterruptible power supply (UPS)- if the power cord is accidentally pulled out of the socket, replacing it quickly may cause no harm.
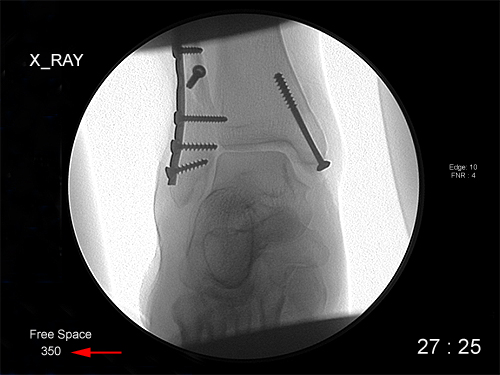
Tip 11. Check Hard-Drive Space Before Starting a New Procedure
You can never be sure how long an operation will take. It is hard to imagine what would be more painful- the ever increasing size of your bladder, or the pain of embarrassment when you ask to stop the operation while you go to the toilet.
Tip 12. Check That the Surgeon is Operating on the Correct Side
</a>If you are using an image intensifier with a hard drive, check that you have plenty of hard drive space left before you start. It can be very awkward to stop a theatre case while you free up some hard drive space on your image intensifier.
Obviously, if you are using a non-digital image intensifier, this will not be an issue.
Tip 13. Watch the Surgeon's Eyes When Screening
</a>It is sound practice to have a good look at the patient's old imaging. You can often pick up points that will help during the operation. The operation may also make more sense to you if you understand the patient's history and the nature of their injuries.
Importantly, check that the surgeon is operating on the correct side of the patient. Once the scrub nurse has prepared one side of the patient for surgery, the surgeon will tend to assume that is the affected side.
In short, the surgical team should aim to perform the correct operation, on the correct side of the patient, on the correct patient.
Beware, errors are made.
Tip 14. Use a Sequence Acquisition When Appropriate
</a>This is not a matter of romance- it's a radiation protection issue. If it is normal procedure for the radiographer to initiate fluoroscopy, or if the surgeon has the fluoro' peddle, this is still good practice (this is a debatable point- researchers have reported conflicting findings). What you are trying to minimise is the time that the surgeon spends screening when he/she is not looking at the image. It is not uncommon for the surgeon to ask you to initiate fluoroscopy but not tell you to stop. They are simply concentrating on what they are doing and forget that they have initiated fluoroscopy.
It helps if you understand what they are doing at every stage of the operation. This will help you to decide whether the surgeon has averted their eyes momentarily from the image (and wants you to keep screening) or whether they have simply forgotten to tell you to stop screening.
Tip 15. Be Careful When Moving the C-arm
</a>Modern mobile digital Image Intensifiers are able to store images in a run or sequence. You set the relevant parameters such as capture rate, and the images will be stored in a sequence (it's a bit like an animated GIF).
I see this as having several advantages. Firstly, my understanding is that the Image Intensifier is performing screen capture and there is no cost in terms of increased radiation dose to the patient.
Secondly, you are able to record dynamic information. This can be particularly useful in cases such as ERCP or Laparoscopic Cholangiogram. If there appears to be a stone in the CBD you can play the sequence back to the surgeon and see if the stone acts more like an air bubble or a stone.
- does it deform in shape
- does it divide in two when it reaches the hepatic ducts
- does it float up hill or down hill
Another less obvious use is when the surgeon wants to assess the stability of a joint following ORIF.
Tip 16. You are Responsible for your Students
</a>It is possible to do harm when you are moving the C-arm.
When you are assisting with a hip operation, the surgeon will usually want to see that anatomy in the lateral projection. The image intensifier is usually set up to roll under the operating table for the lateral projection. The first time you roll the C-arm into the lateral projection be very careful. Go slowly and ask the surgeon if everything is " Ok over there".
Similarly, you can fracture a patient's pelvis when lowering the C-arm. Also watch the anaesthetist who is raising or lowering the operating table when the C-arm is in place.
Tip 17. Use Equipotential Earthing for Cardiac Cases
Qualified radiographers will generally be held accountable for the students under their instruction. I have seen a scrub nurse drop a pair of forceps- the radiography student picked them up and put them back on the sterile tray for her. It is worth emphasizing to a student radiographer who is entering the operating theatre for the first time the following three points.
- If you feel unwell, leave the theatre immediately
- If you feel faint, back up to a wall and slide down it until you are sitting on the floor
I was once told that the true measure of a surgeon's ability to train a student lies in their preparedness to let that student operate on them. We should think of student radiographers in the same way- we train them to a level that we would be confident to be their patient.
Tip 18. Don't Clean the Image Intensifier During Open Surgery
You may have wondered why your image intensifier has a separate earth lead when it is earthed through the plug. This extra earthing wire can be used during cardiac cases (pacing wires, defibrillator insertion, ablation etc) when equipotential earthing is required. If all of the equipment in the operating theatre is earthed to the same earth point, the grounding of the equipment will be identical. This can assist with electrical safety and avoid static discharge during surgery.
Tip 19. Distance, Shielding, Time
It can be tempting to do a little bit of cleaning of the image intensifier during the operation. This is inadvisable. If you are using a spray bottle, the aerosol will potentially enter an open wound and cause infection.
This is not to suggest that the image intensifier does not need cleaning between cases. If you want to see what the theatre staff look like when they are upset, try wheeling a blood covered image intensifier into an operation.
Cleaning the image intensifier can be more difficult and time consuming than it looks. There can be crevices that are hard to access. Also, you will need to turn the c-arm upside down to be sure that the image intensifier is completely clean.
Tip 20. What if I feel like I am About to Faint?
The three basic principles of radiation protection are
- distance,
- shielding
- time.
Distance is often overlooked as a radiation protection technique. This is possibly related to a notion that if you are wearing a lead gown, you are receiving no ionising radiation. Of course, the lead gown is not covering your entire body. In keeping with the ALARA principle, it is good practice, where appropriate, to move away from the image intensifier as far as possible.
It is also worthwhile considering other radiation protection issues. eg.
- When should you use overcouch techniques and when should you use undercouch techniques?
- What is the shape of the radiation scatter cloud from an image intensifier- where is it safest to stand?
If you feel like you are going to faint, back up to a wall and slide down it. You are not the first person to faint in an operating theatre and you will not be the last. Even a hardened radiographer can feel faint in certain circumstances- e.g.
- if you are dehydrated
- if the operative theatre is very hot
- if the operation is very long
- if you are standing for a long period wearing a lead gown
I find it useful during long theatre cases to find a seat and take the weight off my feet. Check with your departmental and theatre rules on this one.Fainting doesn't have to be a drama!
Jeremy Enfinger has some notes on where to centre for surgical procedures at his website <a class="external" href="http://bloggingradiography.blogspot.com/search?updated-min=2007-01-01T00%3A00%3A00-05%3A00&updated-max=2008-01-01T00%3A00%3A00-05%3A00&max-results=36" rel="nofollow" target="_blank">here</a>
....back to the applied radiography home page here