Osgood-Schlatter Disease
Osgood schlatter disease refers to partial avulsion of the tibial tuberosity (anterior surface of apophysis). This page considers all aspects of radiography of Osgood-schlatter disease.
What is Osgood-Schlatter (OSD) disease?
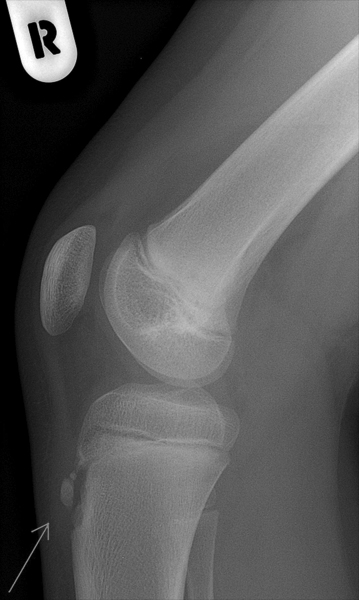
Prominance of the tibial tuberosity's typical of Osgood Schlatter disease.
<a class="external" href="http://1.bp.blogspot.com/_GLm3c6DgPMw/R0Vzm9wCrVI/AAAAAAAABFU/IPWLO0TBlds/s400/os1.jpg" rel="nofollow" target="_blank">http://1.bp.blogspot.com/_GLm3c6DgPMw/R0Vzm9wCrVI/AAAAAAAABFU/IPWLO0TBlds/s400/os1.jpg</a>"Osgood-Schlatter disease or syndrome (also known as tibial tubercle apophyseal traction injury) is a rupture of the growth plate at the tibial tuberosity, and is one of a group of conditions collectively called osteochondroses. The condition is named after the American surgeon Robert Bayley Osgood (1873–1956) and the Swiss surgeon Carl Schlatter (1864–1934), who independently described the disease in 1903. The condition occurs in active boys and girls aged 11-15, coinciding with periods of growth spurts. It occurs more frequently in boys than in girls, with reports of a male-to-female ratio ranging from 3:1 to as high as 7:1. It has been suggested the difference is related to a greater participation by boys in sports and risk activities than by girls.
The condition is usually self-limiting and is caused by stress on the patellar tendon that attaches the quadriceps muscle at the front of the thigh to the tibial tuberosity. Following an adolescent growth spurt, repeated stress from contraction of the quadriceps is transmitted through the patellar tendon to the immature tibial tuberosity. This can cause multiple subacute avulsion fractures along with inflammation of the tendon, leading to excess bone growth in the tuberosity and producing a visible lump which can be extremely painful when hit.
The syndrome may develop without trauma or other apparent cause; however, some studies report up to 50% of patients relate a history of precipitating trauma. In a retrospective study of adolescents, young athletes actively participating in sports showed a frequency of 21% reporting the syndrome compared with only 4.5% of age-matched nonathletic controls. Sinding–Larsen–Johansson syndrome is an analogous condition involving the patellar tendon and the lower margin of the patella bone, instead of the upper margin of the tibia." <a class="external" href="http://en.wikipedia.org/wiki/Osgood-Schlatter_disease" rel="nofollow" target="_blank">(wikipedia)</a>
<embed allowfullscreen="true" height="350" src="http://widget.wetpaintserv.us/wiki/wikiradiography/widget/youtubevideo/20dcffa91ce5e35b2cd353c3c72617b8c13fa559" type="application/x-shockwave-flash" width="425" wmode="transparent"/> <embed allowfullscreen="true" height="350" src="http://widget.wetpaintserv.us/wiki/wikiradiography/widget/youtubevideo/80f099536e24deb506f31cf91963afa1f5289434" type="application/x-shockwave-flash" width="425" wmode="transparent"/> <embed allowfullscreen="true" height="350" src="http://widget.wetpaintserv.us/wiki/wikiradiography/widget/youtubevideo/14b29871c30ca230f6795443c56f1af692af2160" type="application/x-shockwave-flash" width="425" wmode="transparent"/> <embed allowfullscreen="true" height="350" src="http://widget.wetpaintserv.us/wiki/wikiradiography/widget/youtubevideo/3baf0bc1fbbc1b2ed4545c5a7afe81e9ba6a21b8" type="application/x-shockwave-flash" width="425" wmode="transparent"/> <embed allowfullscreen="true" height="350" src="http://widget.wetpaintserv.us/wiki/wikiradiography/widget/youtubevideo/cca95d747bc3c733d169f2c86a60305b25ee54f2" type="application/x-shockwave-flash" width="425" wmode="transparent"/>
Radiography of OSD
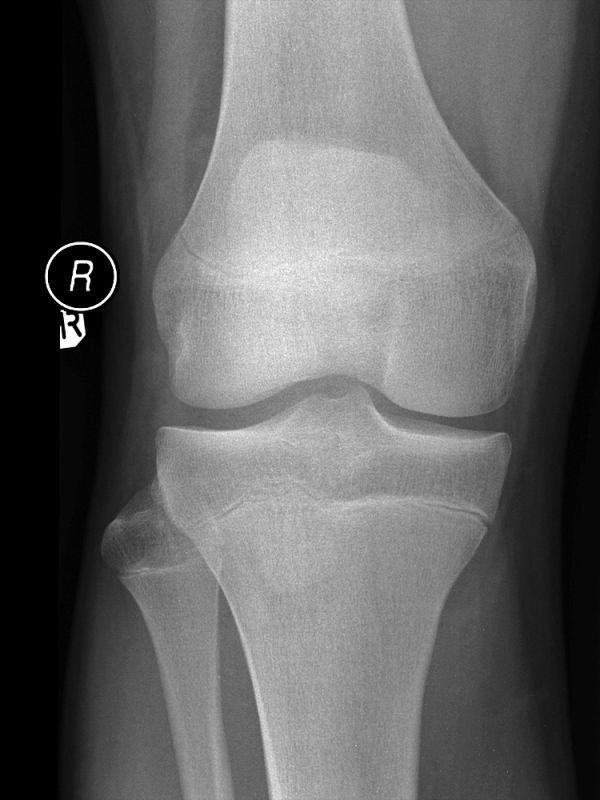
Osgood Schlatter disease is as much a clinical diagnosis as it is a radiographic diagnosis. OSD is type of juvenile traction osteochondritis. (Osteochondritis is a painful condition where the cartilage and bone in a joint is inflamed). The patient's agegroup (more common in late childhood or early adolescence), sex (more common in boys), activity levels (may represent an over use disease) and localised symptoms relating to the tibial tuberosity will often provide a convincing diagnosis. Knee radiography may be requested in patients with suspected OSD. The lateral knee view is the most diagnostically useful view. A fragmented tibial tuberosity is helpful in supporting the diagnosis of OSD but the plain films may appear normal in the patients with OSD. A fragmented tibial tuberosity can also be normal. A bone scan may be useful in confirming the presence of OSD. The greatest utility of plain film radiography may be in excluding alternate diagnoses (infection and tumour).
For patients presenting for acute imaging and follow-up knee imaging of OSD, it is prudent to perform the lateral projection with no knee flexion rather than the recommended 30 degrees. Flexing the knee will subject the patient's tibial tuberosity to a mechanism/force which caused the original injury- that is, the patellar tendon will apply a traction force to the tibial tuberosity (you would do well to adopt the first rule of nursing- do no harm)
Plain Film Appearances
Soft Tissue Swelling
<a class="external" href="http://upload.wikimedia.org/wikipedia/commons/e/e5/Osgood.jpg" rel="nofollow" target="_blank">Source: http://upload.wikimedia.org/wikipedia/commons/e/e5/Osgood.jpg</a>Soft tissue swelling is often the only radiographic evidence of Osgood Schlatter disease on plain film imaging. The AP view is of little assistance in diagnosis OSD. Fragmentation of the tibial tuberosity can be a normal finding.
Avulsion of the Tibial TuberosityPatellar Tendon Thickening
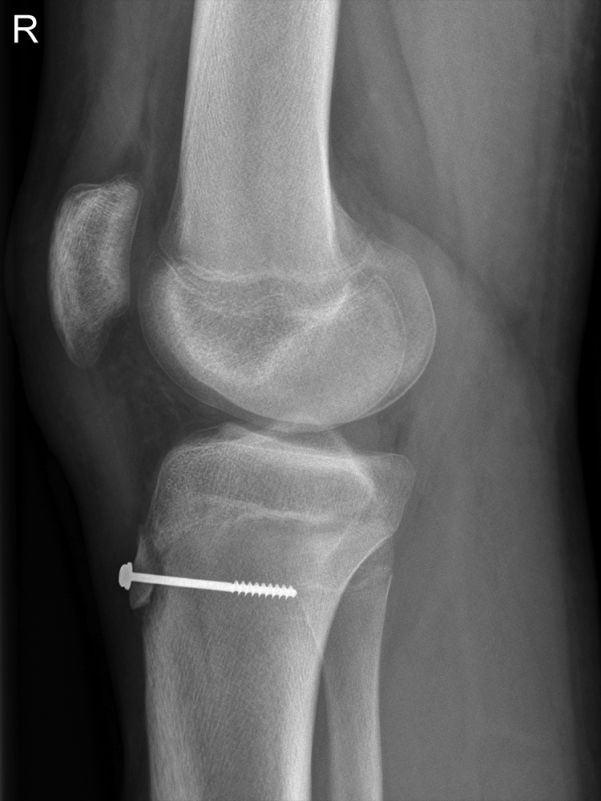
Osgood Schlatters Disease
<a class="external" href="http://upload.wikimedia.org/wikipedia/commons/e/e5/Osgood.jpg" rel="nofollow" target="_blank">
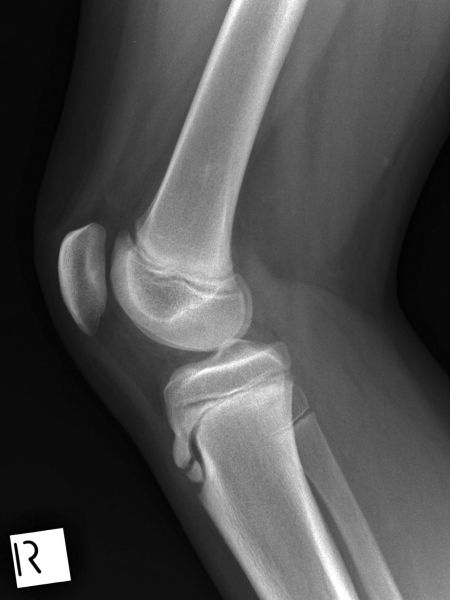
</a>Normal Knee
<a class="external" href="http://upload.wikimedia.org/wikipedia/commons/e/e5/Osgood.jpg" rel="nofollow" target="_blank"></a>
This child has Osgood Schlatter's disease on the right. Comprae the patellar tendon of this affected knee wiith the patellar tendon of his normal knee (above right) The patellar tendon on the normal side shows relatively consistent thickness.
Fragmented Tibial Tuberosity
<a class="external" href="http://upload.wikimedia.org/wikipedia/commons/e/e5/Osgood.jpg" rel="nofollow" target="_blank">
</a>This 13 year old boy presented to the Emergency Department with a sore left knee following a sports injury. He was examined and found to be tender in the region of this Left patellar tendon. He was referred for left knee radiography. The tibial tuberosity is fragmented (white arrow). Whilst this is not diagnostic for Osgood Schlatter's disease (OSD), the appearance is consistent with OSD.
Note the tickening of the patellar tendon with a possible fluid collection between the patellar tendon and the proximal tibial epiphysis (black arrow). Hoffer's fatpad demonstrates mixed fat and fluid density consistent with an acute injury.
Patella alta noted
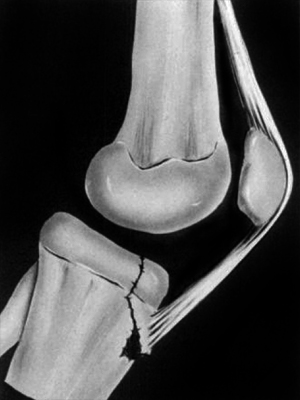
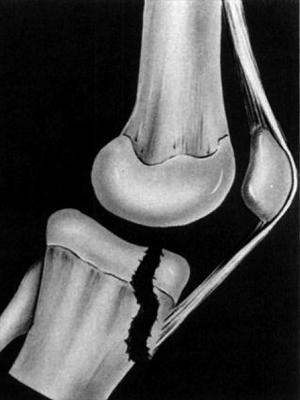
Case Study 1Osgood Schlatter disease can be a predisposing factor in cases of avulsion of the the tibial tuberosity.
Type I Fracture
<a class="external" href="http://www.ejbjs.org/cgi/reprint/53/8/1579.pdf" rel="nofollow" target="_blank">WILLIAM L. HAND, CHARLES R. HAND and A. WILLIAM DUNN
Avulsion Fractures of the Tibial Tubercle
J Bone Joint Surg Am. 1971;53:1579-1583.</a>Type II Fracture
<a class="external" href="http://www.ejbjs.org/cgi/reprint/53/8/1579.pdf" rel="nofollow" target="_blank">WILLIAM L. HAND, CHARLES R. HAND and A. WILLIAM DUNN
Avulsion Fractures of the Tibial Tubercle
J Bone Joint Surg Am. 1971;53:1579-1583.</a>Type III Fracture
<a class="external" href="http://www.ejbjs.org/cgi/reprint/53/8/1579.pdf" rel="nofollow" target="_blank">WILLIAM L. HAND, CHARLES R. HAND and A. WILLIAM DUNN
Avulsion Fractures of the Tibial Tubercle
J Bone Joint Surg Am. 1971;53:1579-1583.</a>In Type-I injuries, the tubercle is hinged upward without displacement at its proximal base. The Type-lI injury has a smaller portion of the tubercle avulsed, but it is retracted proximally. The articular surface is not involved. Type-Ill injuries are more severe and extend across the articular surface. There is displacement of the fragment and often comminution.
Case Study 2
... back to the Wikiradiography home page
... back to the Applied Radiography home page