Nasogastric Tube Position Confirmation
Chest radiography for nasogastric tube (NGT) position is commonplace in many hospitals. The aim is to positively confirm that the exit hole(s) of the NGT is/are within the gastrointestinal tract (usually the stomach). If the longer nasoenteric tube is used, the objective is to place the tip of the tube past the pylorus into the jejunum. This tip position bypasses the regulatory function of the pylorus and delivers nutrition/therapeutic agents directly into the jejunum. Even if a nasoenteric tube has its tip in the stomach, if there is enough tubing in the stomach, normal peristalsis will tend to propel it distally (but not always).
The importance of establishing the position of the NGT cannot be understated. A patient who is fed or administered drugs via a malpositioned NGT can have very poor outcomes including<a class="external" href="http://www.theage.com.au/articles/2004/08/23/1093246442769.html?from=storylhs" rel="nofollow" target="_blank"> iatrogenic death</a>. X-ray confirmation of NGT position is not practised in some centres- the position of the tip of the NGT is assessed by drawing back gastric contents and testing with ph paper.
Insertion Technique
There is no shortage of videos on <a class="external" href="http://youtube.com/" rel="nofollow" target="_blank">Youtube</a> covering the subject of NGT insertion. Here's a few of them
<embed align="left" height="350" src="http://widget.wetpaintserv.us/wiki/wikiradiography/page/Nasogastric+Tube+Position+Confirmation/widget/unknown/4a46b6de2990d5982bd3fa0de2261fef197229e1" type="application/x-shockwave-flash" width="425" wmode="transparent"/> <embed height="350" src="http://widget.wetpaintserv.us/wiki/wikiradiography/page/Nasogastric+Tube+Position+Confirmation/widget/unknown/e175629317767d00c210d2b8ab39b1aabf1070a2" type="application/x-shockwave-flash" width="425" wmode="transparent"/> <embed height="350" src="http://widget.wetpaintserv.us/wiki/wikiradiography/page/Nasogastric+Tube+Position+Confirmation/widget/unknown/f88387efd7c499a783c60e43ea14a078d131abbd" type="application/x-shockwave-flash" width="425" wmode="transparent"/> <embed height="350" src="http://widget.wetpaintserv.us/wiki/wikiradiography/page/Nasogastric+Tube+Position+Confirmation/widget/unknown/fa9370c09b3cf3144b6eccc201cfc77239939f71" type="application/x-shockwave-flash" width="425" wmode="transparent"/> (Note: Youtube videos are displayed at lower resolution when 'hot-linked'. Click on the bottom right corner of the video and it will open at full resolution.) (Note: Youtube videos are displayed at lower resolution when 'hot-linked'. Click on the bottom right corner of the video and it will open at full resolution.)
<a class="external" href="http://www.tomwalsham.com/News/4396273.stm_files/_40978923_nasal_tube_inf203.gif" rel="nofollow" target="_blank">
</a>
Select a tube <a class="external" href="http://www.joannabriggs.edu.au/protocols/protnasotube.php#anchorBackground" rel="nofollow" target="_blank">size and type</a>.
Explain the procedure to the patient and obtain consent from the patient to proceed.
Sit patient upright for optimal neck/stomach alignment
Wash hands and don disposable gloves.
NGTs are generally inserted via the nostril (...by definition). Alternatively, an orogastric tube can be used - this tube is inserted via the patient’s mouth into the stomach. It is worth asking the patient which nostril is more patent. A deviated nasal septum, polyps or other pathology may suggest one nostril will be more patent than the other. It can be helpful to check nostrils for patency by asking patient to occlude one nostril and breathe normally through the other. Select the nostril through which air passes most easily. Alternatively, ask the patient to blow their nose into a tissue.
Close the access port on the NGT. It is amazing how often the contents of a patient's stomach are deposited on their pillow because the access port was left open.It is good practise to do a quick assessment of whether the NGT is long enough for the patient. Viasys Healthcare recommend the following technique in their instructions for inserting an Enteral Feeding tube with stylet.
"Place the exit port of the tube at the tip of the nose. Extend tube to earlobe, then to xiphoid process. ...Use the printed centimeter marks on the tubes to aid intubation and check for tube migration.
If there are no centimetre marks on the tube, tape could be placed on the tube to mark the desired insertion length. Lubricate the tip of tube (at least 1-2 inches) with water-soluble lubricant. Apply topical analgesic to nostril and oropharynx or ask patient to hold ice chips in his or her mouth for several minutes.
Insert the tube into nostril while directing the tube downward and backward. Patient may gag when the tube reaches the pharynx. Instruct the patient to touch his or her chin to chest. If the patient is conscious and compliant, he/she is instructed to swallow during the insertion of the NGT. Swallowing small sips of water may enhance the passage of the tube into the oesophagus. The swallowing action and peristaltic waves assist the NGT to enter the oesophagus and also assist its passage to the stomach. Advance the tube in a downward-and-backward direction when the patient swallows. Stop when the patient breathes. If gagging and coughing persist, check placement of tube with a tongue blade and flashlight. Keep advancing tube until tape marking is reached. Do not use force. Rotate the tube if it meets resistance.Apply tincture of benzoin to tip of nose and allow to dry. Secure tube with tape to patient’s nose. Be careful not to pull the tube too tightly against nose.
It is very helpful if the doctor/nurse leaves the NGT's luminal wire (stylet) in place until the confirming radiograph has been performed. Once that stylet is removed, it should not be reinserted. I have heard it suggested that if the wire is removed from the NGT, contrast medium could be injected down the NGT to help identify its position. Air injected down the NGT has also been suggested as a contrast agent to inflate the stomach. Both techniques are not recommended unless it has been proven that the NGT is not in the patient's pleural space or anywhere else that it can cause harm.
NGT should be looped and taped to patient or secured at the patient's nose with suitable adhesive tape.
You can estimate the amount of NGT inside the patient by examining the length of NGT outside the patient. If you keep sample NGTs in you radiography suite, it might be worth checking whether the tip of the NGT could even conceivably be located in the stomach. I have had patients referred for chest radiography for NGT position despite the fact that almost the entire length of the NGT is hanging out of the patient's nose!
<a class="external" href="http://books.google.com.au/books?id=M4HwH5IxfToC&pg=PA665&lpg=PA665&dq=nasogastric+tube&source=web&ots=yeOWHPsn6y&sig=CI19u7HfMIodO2kY9nO6mj9FgsQ&hl=en&sa=X&oi=book_result&resnum=4&ct=result#PPA669,M1" rel="nofollow" target="_blank"></a>
Complications
- Patient non-consent to procedure
- Anticoagulation or coagulopathy
- Basilar skull fracture
- Nasal or other trauma that might affect insertion
- Sinus surgery
- Recent sphenoidal or transsphenoidal surgery
- Nasopharyngeal tumours
- Oesophageal varices
- Recent oesophageal surgery
- Oesophageal stricture
- <a class="external" href="http://www.radswiki.net/main/index.php?title=Intracranial_nasogastric_tube" rel="nofollow" target="_blank">Intracranial Insertion</a>
- Pleural Space Insertion
- Lung insertion
- bleeding
- knot forms in NGT
Radiographic Technique
- The radiographic technique for NGT placement confirmation is most commonly erect or supine, AP or PA chest radiography. The technique is modified to take into account that a successfully positioned NGT will be visualised below the diaphragm. Radiographers will commonly place the cassette in the portrait position rather than the landscape position to ensure that the subdiaphragmatic anatomy is included.
- There might seem like a prima facie case for abdominal radiography, or radiography centred on the diaphragm, rather than chest radiography. However, the NGTs do not always end up in the desired position. In some cases the NGT can become coiled up in the pharynx. If you don't include the pharynx, the result can be puzzling- where did the NGT go?
- A penetrated exposure is often required to visualise the tip of the NGT below the diaphragm, particularly when using non-digital equipment. Marking/annotating a radiograph as "penetrated" is prudent in that the image might otherwise be interpreted as inadvertently overexposed (read bad radiography).
- Digital radiography is generally more effective in demonstrating the position of the NGT because of its larger dynamic range.
- It has also been suggested that supine radiography is more effective in demonstrating the NGT position than the AP sitting chest position. The reasoning is that in the AP sitting position, the abdominal tissues are not as "stretched out" and will therefore tend to be underexposed.
- Patients can be referred for NGT insertion under fluoroscopic control. These are commonly patients who have had multiple 'blind' attempts at NGT insertion in the ward. These NGT insertions are frequently difficult insertions where fluoroscopic guided insertion provides much greater chance of success. A fluoroscopic guided NGT insertion is also arguably safer for the patient and should result in a lower risk of malposition and complication.
<embed allowfullscreen="true" height="350" src="http://widget.wetpaintserv.us/wiki/wikiradiography/widget/youtubevideo/e694b9352aa8195c346f4970f84ae173a9ee3438" type="application/x-shockwave-flash" width="425" wmode="transparent"/> This is a fluoroscopic guided NGT insertion on an 81 year old lady who had suffered a recent stroke and was unable to be fed orally. The procedure was undertaken using a C-arm DSI fluoroscopic unit. The C-arm machine has considerable advantage over a non-C-arm unit in that the insertion of the NGT can be followed closely with PA and lateral fluoroscopic surveillance without the patient moving from the supine position.
(Note: Youtube videos are displayed at lower resolution when 'hot-linked'. Click on the bottom right corner of the video and it will open at full resolution.)
The Marginal Position
The tip of the NGT can sometimes appear to be just within the fundus of the stomach. It can be tempting to accept the position of the NGT, particularly when there have been multiple attempts at insertion. This is very risky. Consider the NGT position shown below
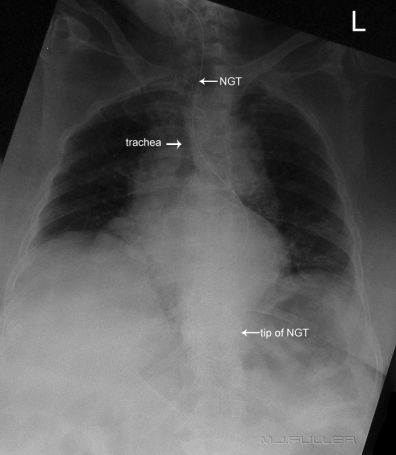
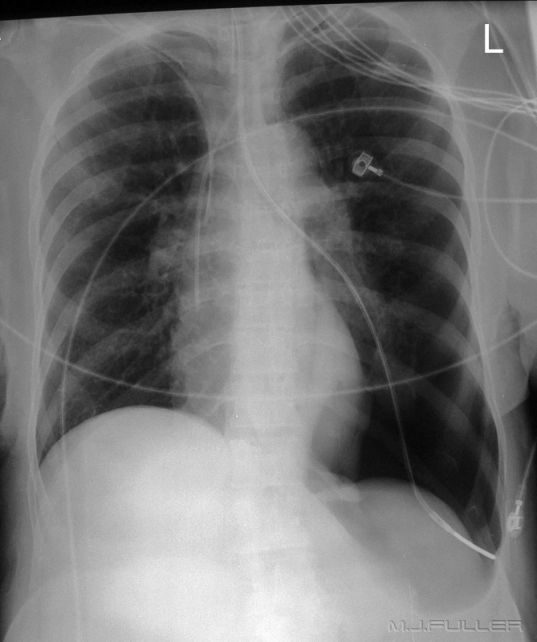
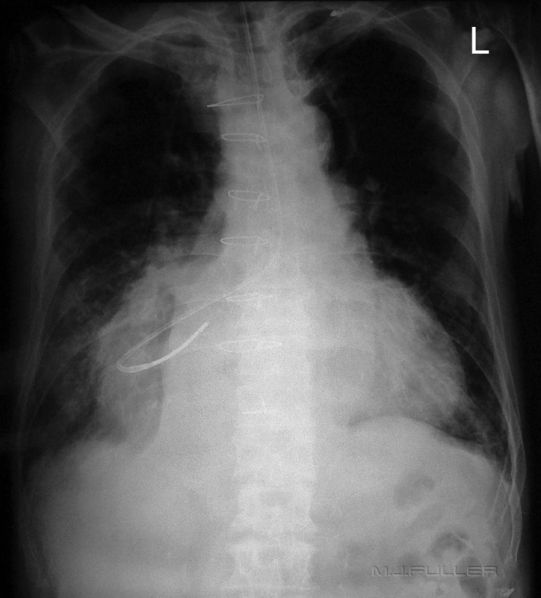
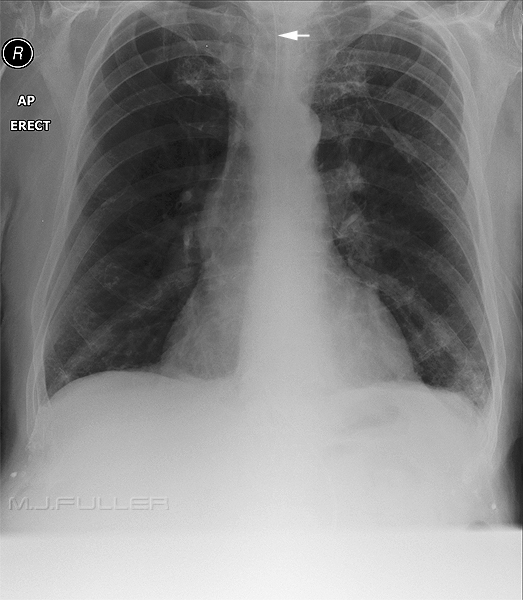
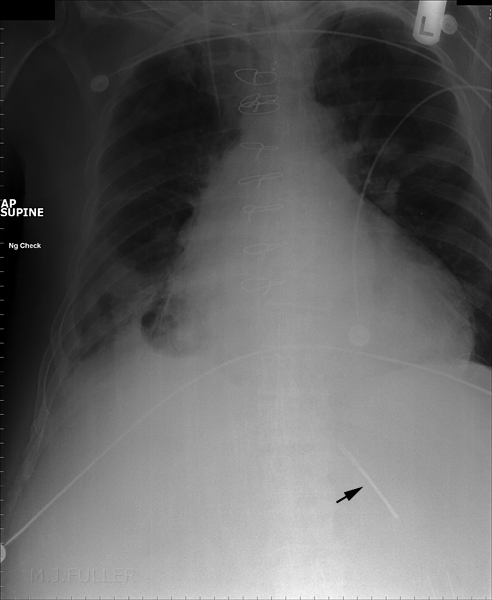
Case 1
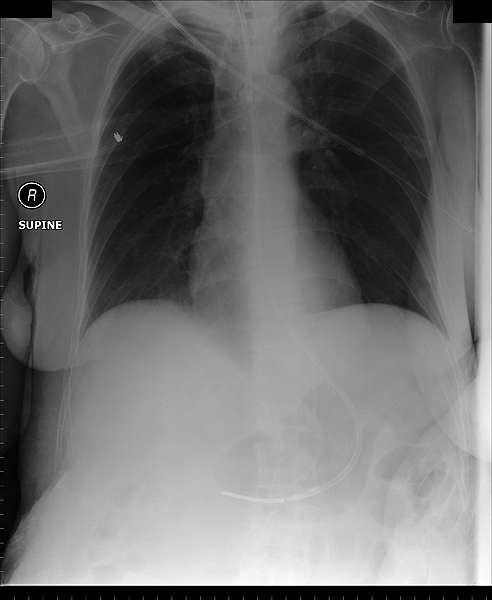
This NGT is in a normal position in the stomach.
Case 2
<a class="external" href="http://intensivecare.hsnet.nsw.gov.au/current/community/equipment/ngt" rel="nofollow" target="_blank"> </a>
<a class="external" href="http://intensivecare.hsnet.nsw.gov.au/current/community/equipment/ngt" rel="nofollow" target="_blank">Source: http://intensivecare.hsnet.nsw.gov.au/current/community/equipment/ngt</a>normal naso-enteric tube position
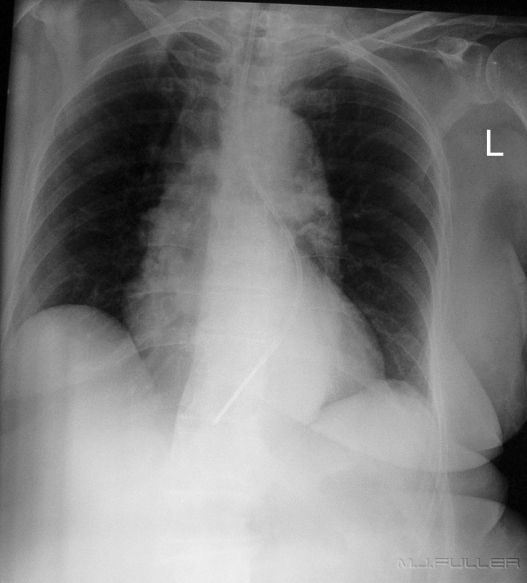
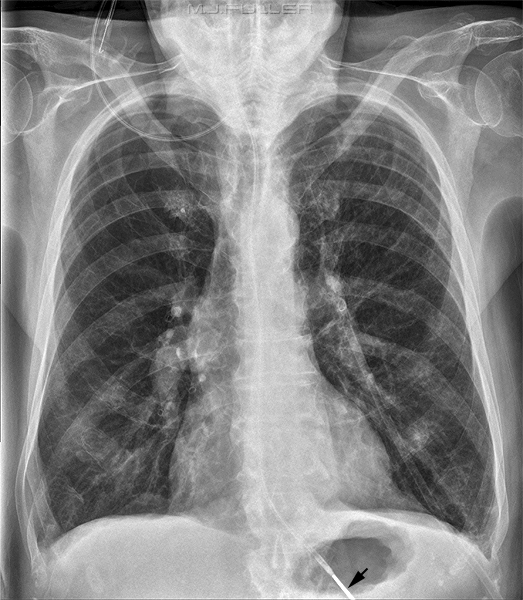
Case 3
| |  |
These images demonstrate one of the most common problems with checking NGT positions radiographically- the NGT is hard to see! If you look closely you can follow the path of the NGT.
With digital systems, post-processing your image can help. It is sometimes difficult to decide whether to widen the window or narrow the window. It is probably wise to concentrate on the tip of the NGT. Whatever post-processing settings show the tip should be used. It is also good practice to produce 2 images from the one exposure: One image can be post-processed to highlight the lungs/heart (a normal CXR setting) while the other is just about the NGT position(black and contrasty).
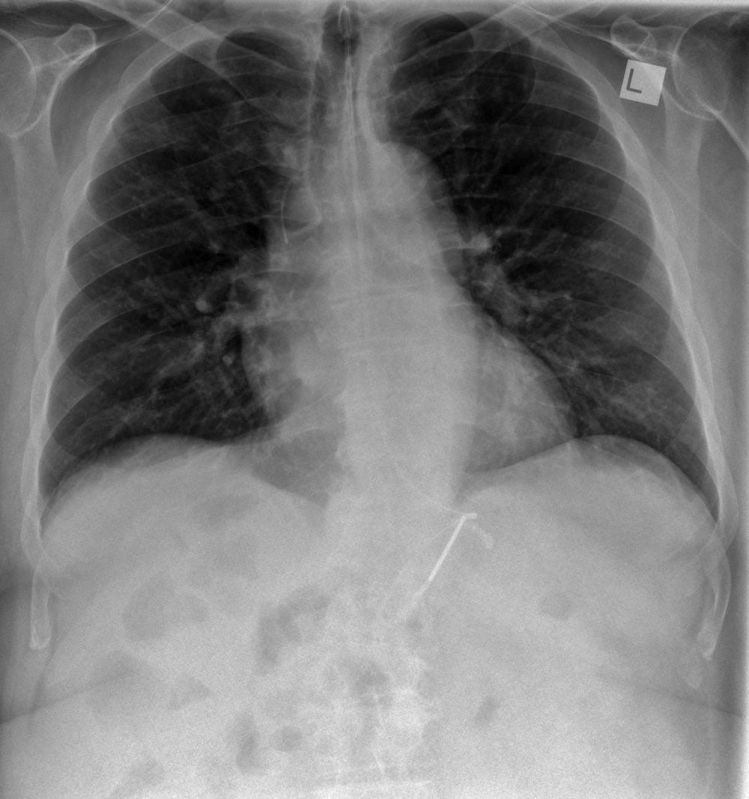
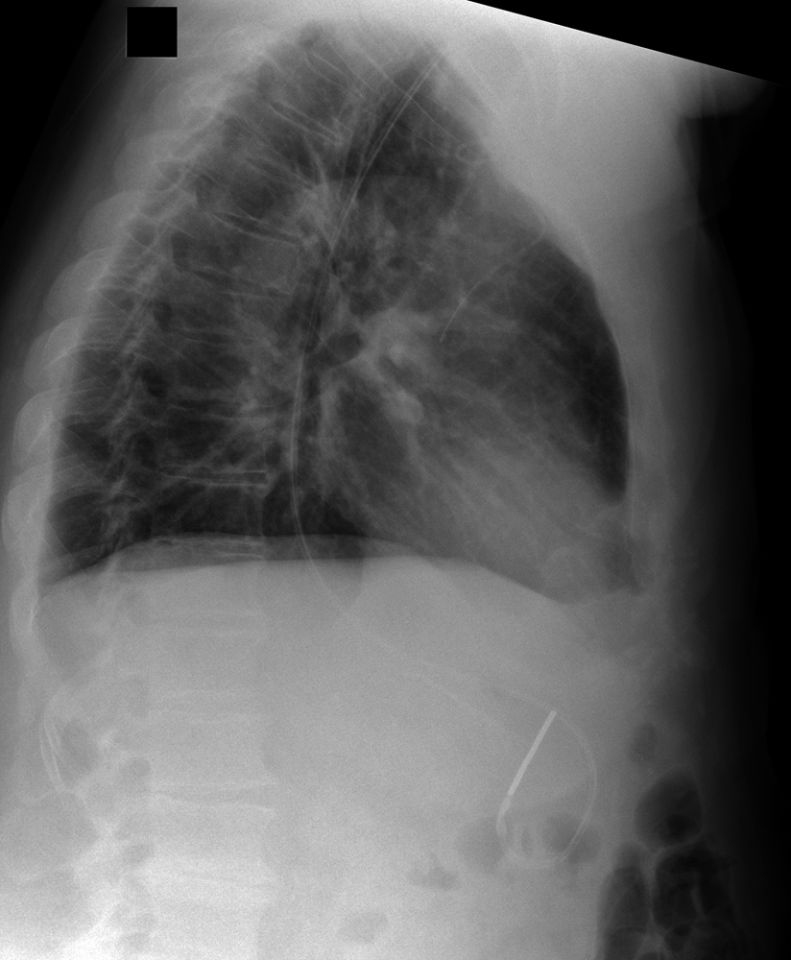
This patient's NGT takes a tortuous course with the tip resting in an indeterminate position. On the AP chest image, it does not appear that the NGT is within the patient's airway. It was considered prudent to perform a lateral chest X-ray examination to provide additional confirmation as to the course of the NGT. The lateral chest image demonstrates that the NGT is posterior to the airway and is likely to be within the oesophagus. The lateral projection also provides additional information about the tip position in relation to the fundus of the stomach.
Care must be taken to ensure that there is enough NGT in the stomach to be sure that the side holes of the NGT are not in the oesophagus.
Inverting a digital image (black on white) can help to visualise a NGT.
Case 4
| | The NGT appears to be following the trachea and the left main bronchus. It is likely that the tip of the NGT has entered the left main bronchus and then deviated down a posterior bronchus into the left lower lobe. An alternative explanation is that the NGT is within a tortuous oesophagus. Regardless of its course, its final tip position is unacceptable |
Case 5a
| | The NGT can be seen to deviate down the left main bronchus. It then appears to reflect off a bronchial division and then take a course down the right main bronchus, possibly into the right middle lobe (bronchus intermedius). |
Case 5b
| | This makes a matching pair with the NGT position shown above. The NGT has entered the RMB then deflected backwards with the tip positioned in the LMB. |
Case 6
| | This NGT has taken a path down the right main bronchus then made its own path through lung parenchyma into the pleural space. This NGT was removed from the pleural space and replaced with an underwater sealed drain (UWSD) which was inserted percutaneously. |
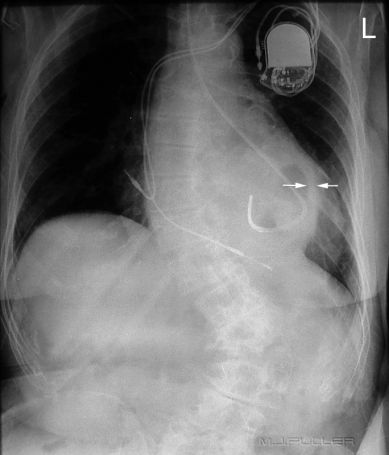
Case 7
| |  |
This patient has a hiatus hernia. The nasogastric tube has entered the hiatus hernia without passing further into the non-herniated subdiaphragmatic stomach. The arrowed structure is likely to be the stomach wall. The lateral projection assists in confirming the presence of the hiatus hernia and the position of the NGT within the hiatus hernia. (note; the diaphragm demonstrated on the lateral view is the right hemidiaphragm)
It is common for NGT insertions to fail in patients with a hiatus hernia. Rather than undertake multiple attempts at insertion, it can be prudent to insert the NGT under fluoroscopic guidance. As a radiographer it is in your interests, the interests of the patient, and the doctor’s interests to offer this service when appropriate. The usual 'on balance' considerations of radiation dose, patient safety and other relevant practical considerations apply.
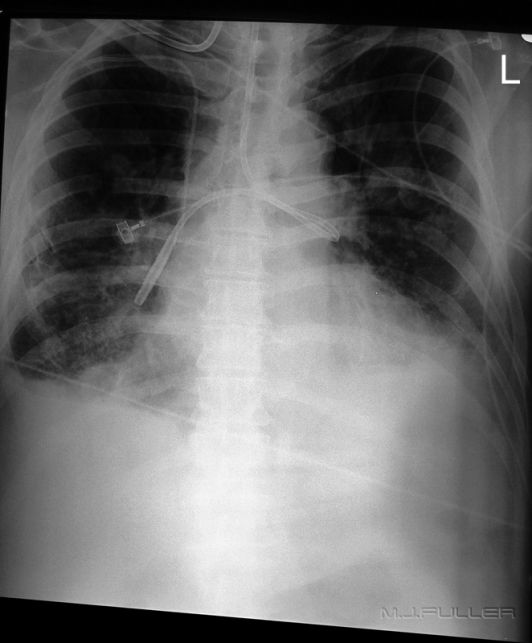
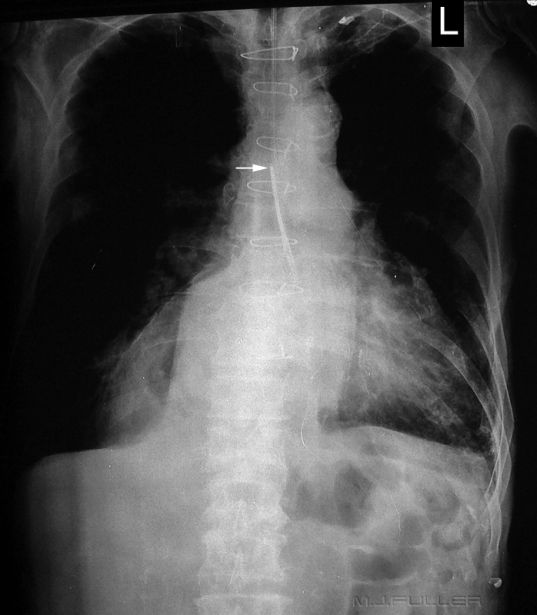
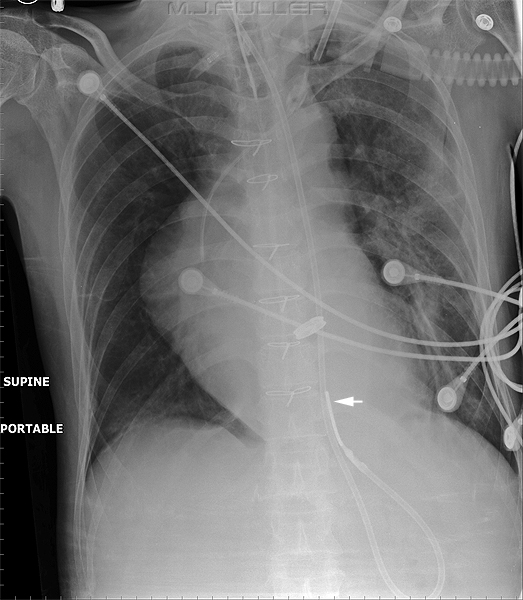
Case 8
| | This patient has a NGT that has passed down the trachea rather than the oesophagus. The NGT has then deflected into the left main bronchus before being pushed through lung parenchyma and the visceral pleura into the pleural space. The mantra for inserting NGTs is definitely not "... just keep pushing". The result of this insertion is a left sided pneumothorax. This is supported by the deep sulcus sign that can be seen at the left lung base. |
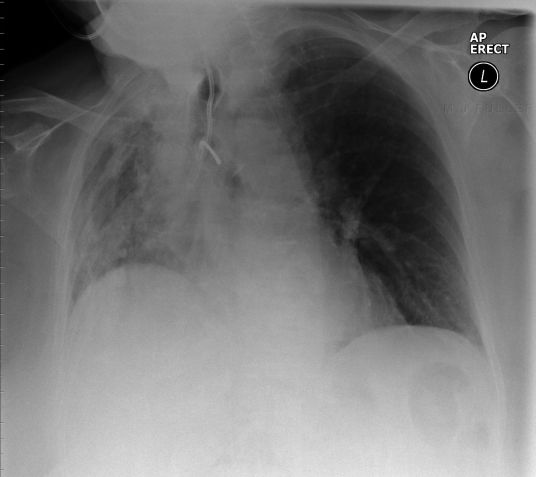
Case 9
| | At a cursory glance, this patient's NGT appears to have passed down the trachea and deviated down the right main bronchus. A more plausible explanation is that it has passed through the oesophagus and come to rest in a large hiatus hernia. A lateral view is likely to demonstrate its true position. |
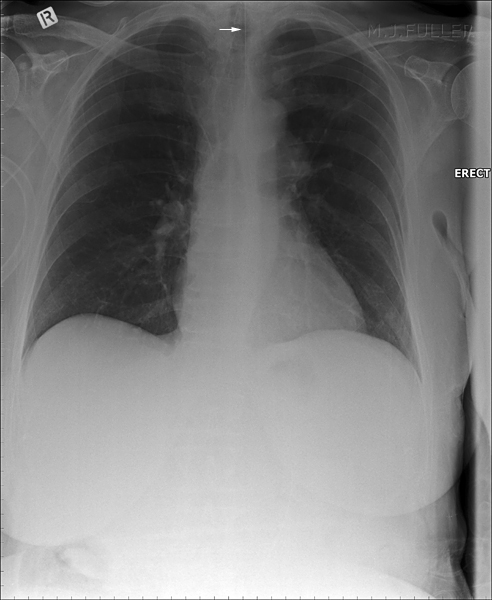
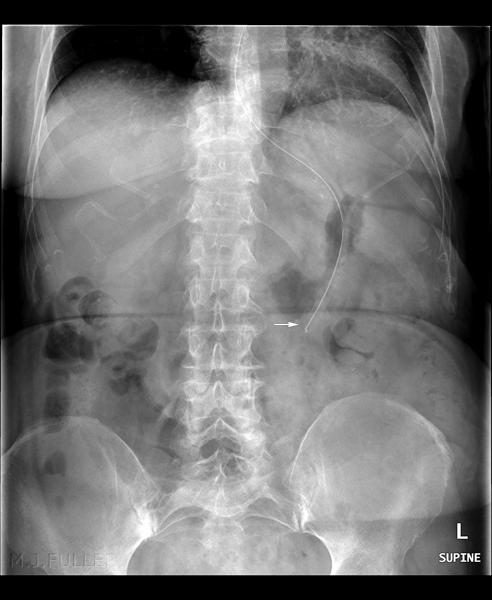
Case 10a
This patient has a NGT that has either reflected and doubled back or has had its tip caught on the way down. The NGT is not in the airway. The patient appears to have a large hiatus hernia and the NGT may have reflected at the level of the gastro-oesophageal junction (GOJ). The GOJ is in the thoracic cavity in this patient.
The tip of the NGT is marked with a white arrow
Case 10b
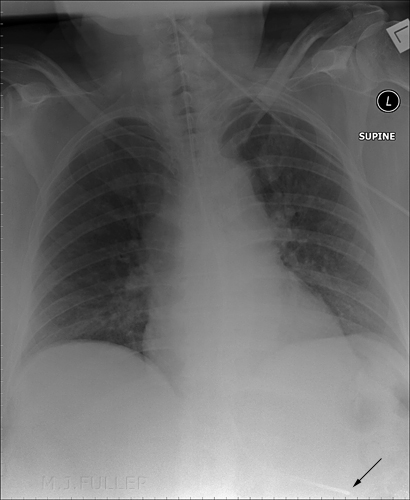
Same Patient
A new NGT has been inserted. Once again the NGT does not appear to be within the right main bronchus. The NGT is likely to have entered the hiatus hernia.
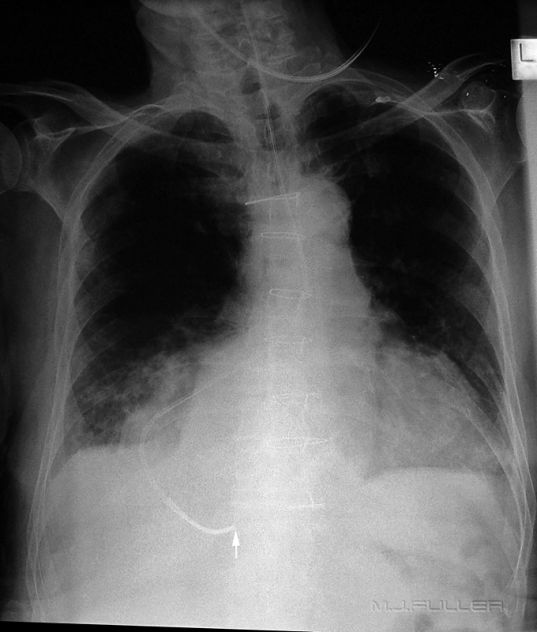
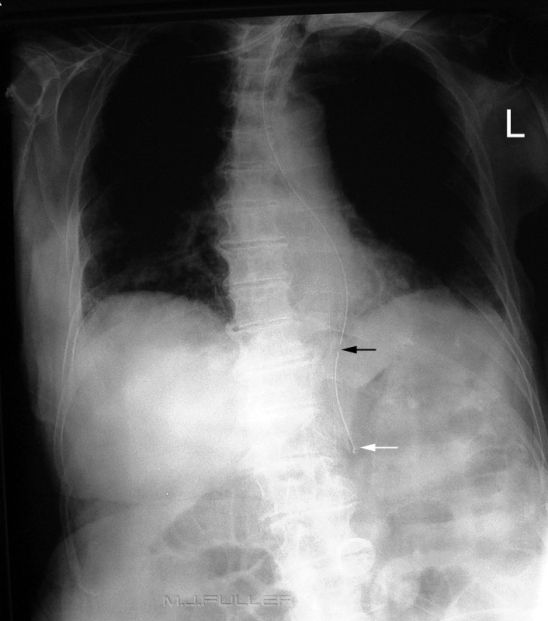
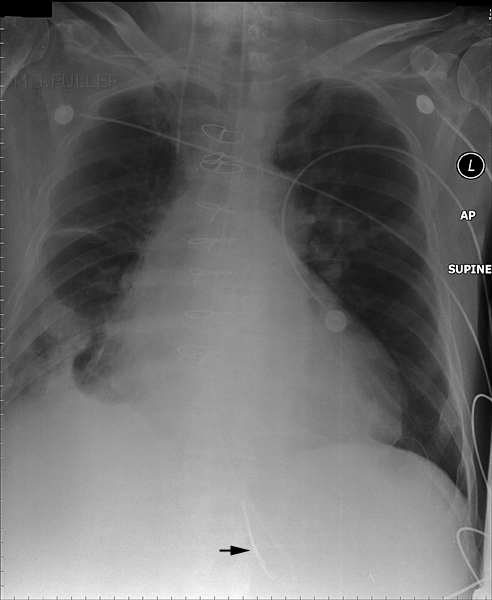
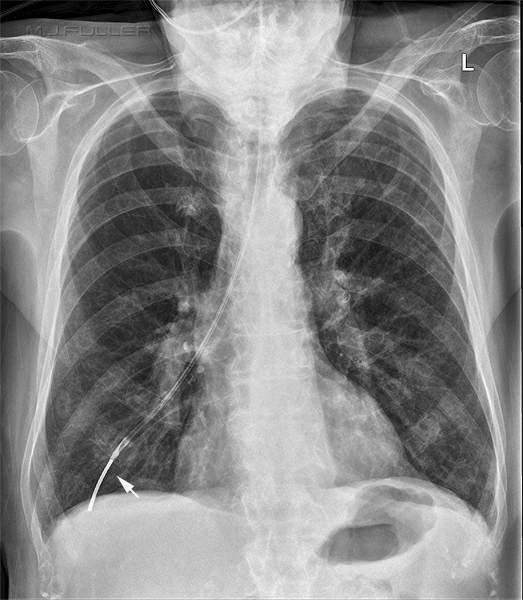
Case 11
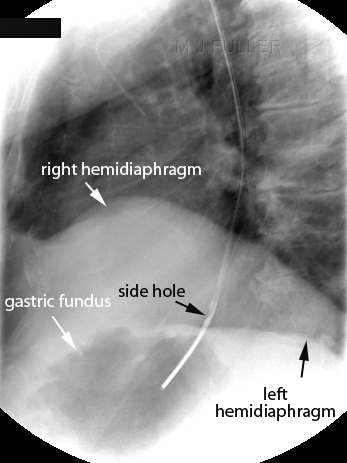
The NGT is likely to have passed down a tortuous oesophagus. The tip of the NGT is probably within the fundus of the stomach (white arrow). The side hole (black arrow) may be within the oesophagus. This is an unacceptable position. If the patient is fed via this NGT, the liquid may exit from the side hole into the oesophagus. If there is sufficient fluid entering the oesophagus it can overflow into the patient's lungs. If there is aspiration of the fluid the patient could die
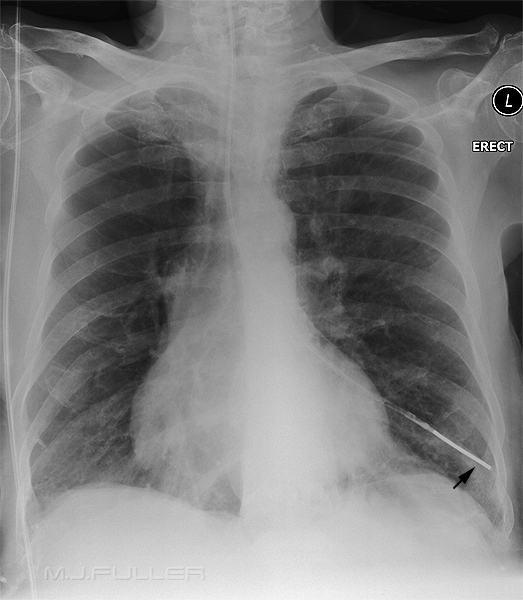
Case 12
| | The tip of the NGT can be seen to be sited in the distal oesophagus. The side hole may be in the fundus of the stomach but it is difficult to be sure. This NGT is unlikely to be manipulated successfully into the correct position and should therefore be removed. |
Case 13a and 13b
These two NGT check images deserved to be presented as a pair.
 |  |
| The tip of the NGT is in the right lower lobe (can you see the button artifact?) | The tip of the NGT is in the left lower lobe |
Case 14
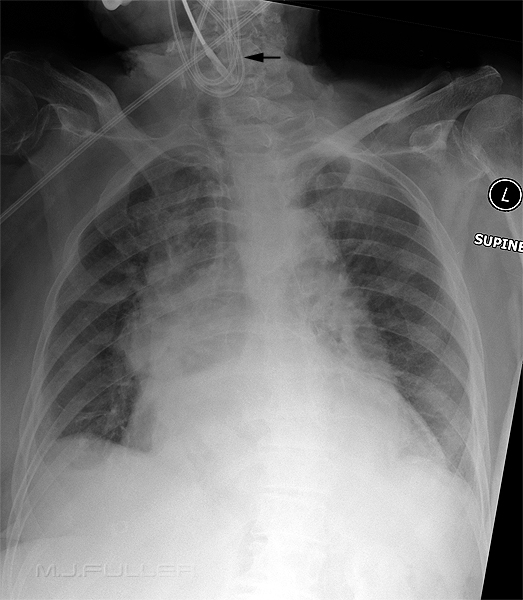
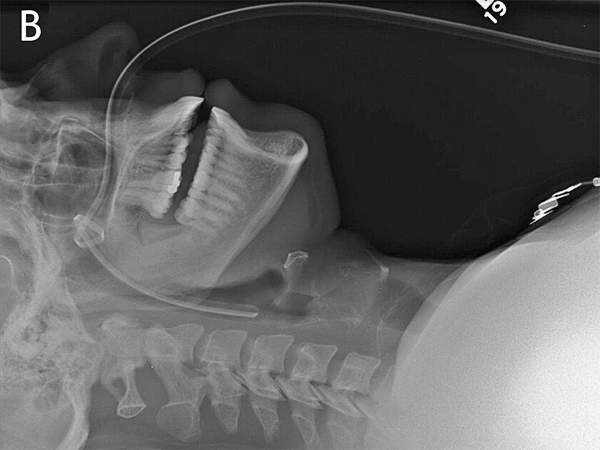
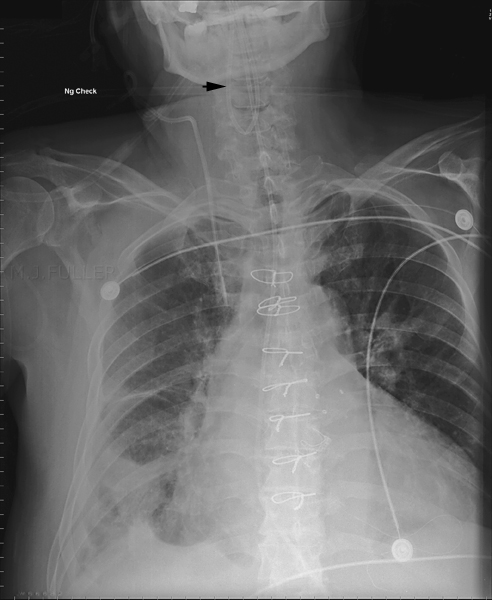
Case 15
The NGT is coiled up in the pharynx. This position can easily be missed if the patient's neck is not included on the image.
Case 16
This NGT is just plain hard to see. The contributing factors may be
- NGT tube is not sufficiently radiopaque
- erect position
- no air in stomach
- under-exposure
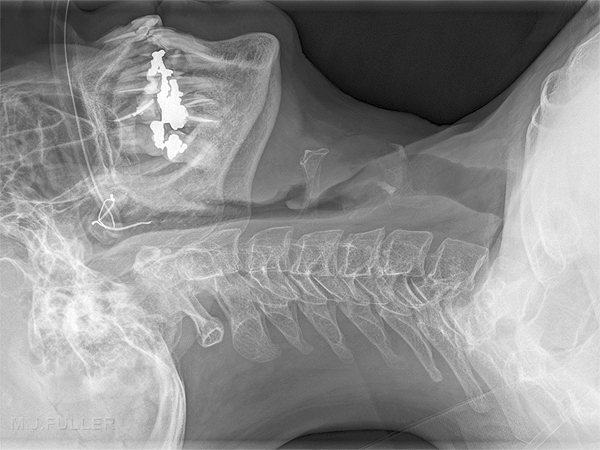
Case 17
This NGT has cleverly manipulated itself into a knot which is positioned in the nasopharynx. The tube was eventually removed through the oral cavity by use of a McGill forceps.
<a class="external" href="http://www.cmaj.ca/cgi/content-nw/full/178/5/568/F118" rel="nofollow" target="_blank">source: http://www.cmaj.ca/cgi/content-nw/full/178/5/568/F118. </a>
The knotting of a NGT is not common. It is possible that knots in NGTs are a result of having too much NGT coiled in the stomach.
Case 18
Same issue as above. NGT was cut near the patient's nose and pulled out through the patient's mouth
Case 19
Case 20
Case 21
Discussion
One of the hidden dangers with NGT-check images is that they are commonplace and the dangers are underestimated. The radiographer should report immediately when a NGT is suspected to be positioned in the lung, or anywhere else that it shouldn't be.
Further Reading
- Metheny N. Measures to test placement of nasogastric and nasointestinal feeding tubes: a review. Nurs Res 1988; 37:324-9.
....back to the applied radiography home page here