Interstitial vs Alveolar Lung Patterns
CautionThis page considers all aspects of the appearances of interstitial and alveolar opacity demonstrated on chest plain film imaging. Radiographers who are able to differentiate alveolar from interstitial lung patterns are operating at a very high level and will find a whole new appreciation of chest radiography. An appreciation of the features of these patterns will prevent you from describing appearances as cloudy, fuzzy etc. You are more likely to gain the respect of your fellow health professionals and impart meaningful information if you can describe an appearance using correct descriptors- e.g "there is widespread coarse interstitial opacity" rather than "the lungs look a bit fuzzy".
Interstitial Opacity on CXR- anatomy, causes and appearances.This is not easy- in fact, this is the difficult end of plain film image interpretation. The interpretation difficulties are as follows
- The appearances can be subtle
- Interstitial patterns can be mixed (linear, reticular, or nodular)
- There can be mixed alveolar and interstitial patterns
- There can be other patterns present (tumour, pleural effusion, atelectasis etc)
- There can be acute on chronic changes.
- The causes of interstitial lung opacity are numerous
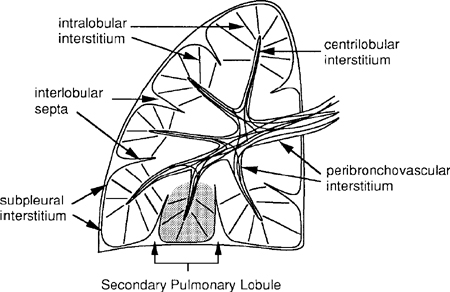
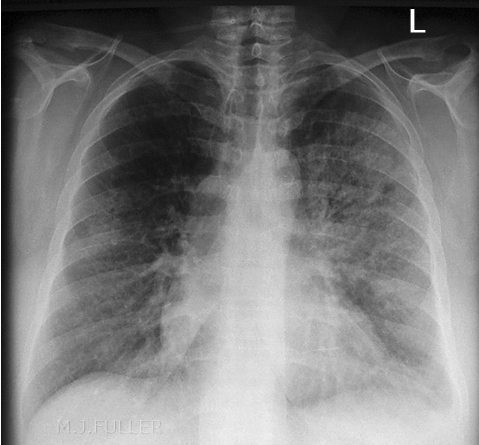
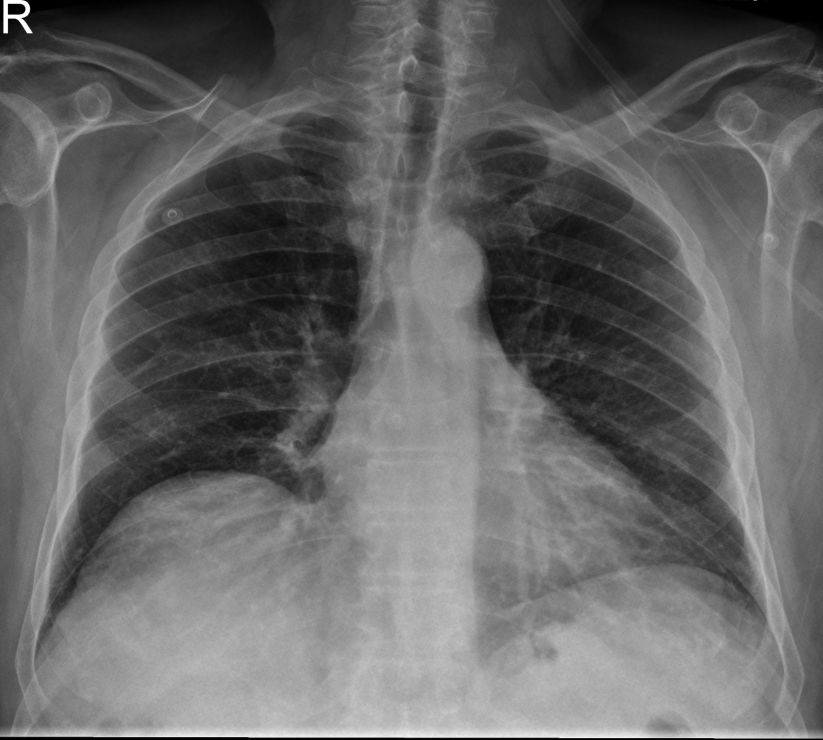
The interstitium of the lung consists of the supporting structures such as pulmonary vessels, bronchi, and connective tissue. On the normal CXR, the visible interstitium consists primarily of the pulmonary vessels, which are most pronounced at the hila, and decrease in prominence towards the periphery (in fact, under normal circumstances, the pulmonary vessels are not visible in the periphery on a CXR because they are too small to resolve at this point). Most lung diseases cause an increase in the radiodensity of the lung, and if this is due to a relative thickening of the interstitium- this will be manifest as increased prominance of the interstitial markings on the CXR. If generalized or diffuse, this will likely appear as a linear or reticular pattern, whereas if localized, it may appear as multiple tiny nodules.
Note that in diseases confined to the interstitium (i.e. sparing the alveoli) the lung will still appear aerated—the basic appearance is of an aerated lung that has too many “markings.” Common causes of this pattern include pulmonary edema, inflammation, fibrosis, and tumour.
The interstitium surrounds bronchi, vessels, and groups of alveoli. When there is disease in the interstitium it manifests itself by reticulonodular shadowing (criss cross lines or tiny nodules or both). The main two processes affecting the interstitium are accumulation of fluid (occurring in pulmonary oedema or in lymphangitis carcinomatosa) and inflammation leading to fibrosis (occurring in industrial lung disease, inflammatory arthritides such as rheumatoid arthritis, inflammation of unknown cause such as cryptogenic fibrosing alveolitis and sarcoidosis).
Quoted from: source unknown
Causes of Interstitial lung opacity
- Common identifiable causes: a) infectious causes, e.g.: non-tuberculous mycobacteria & certain fungal infections
b) occupational causes, e.g.: asbestos & silica
c) drug reactions, e.g.: methotrexate & amiodarone
d) neoplastic causes, e.g.: metastatic cancer, bronchoalveolar cell carcinoma (a form of lung cancer)
e) radiation pneumonitis
f) hypersensitivity pneumonitis
g) rheumatologic diseases(1) systemic lupus erythematosis
(2) rheumatoid arthritis
(3) scleroderma
(4) mixed connective tissue disease
(5) polymyositis
- Diseases of unknown cause, e.g.: sarcoidosis, Langerhan's cell granulomatosis (eosinophilic granuloma; histiocytosis X), lymphangioleiomyomatosis
- Idiopathic pulmonary fibrosisSource: unknown
Causes of Alveolar Opacity
- pneumonitis
- pulmonary contusion
- pulmonary oedema
- Aspiration
The Meaning of the Term 'Consolidation'
One of the unfortunate aspects of the term consolidation is that its meaning can be different depending on who is using the term. When a clinician uses the term consolidation, he/she is usually referring to a consolidation associated with acute pneumonia. Thus, the term consolidation and pneumonia have very similar meaning and are almost used interchangeably. Strictly speaking, the term consolidation does not imply any particular aetiology or pathology. Acute pneumonia is the commonest cause but not the only cause of consolidation. (other causes include chronic pneumonia, pulmonary oedema and neoplasm). Thus when a radiologist has reported a chest X-ray examination and notes the presence of consolidation he/she is simply stating that some of the lung airspace has been replaced by a fluid. Sutton, Textbook of Radiology, 2nd ed.,1975,
<embed height="350" src="http://widget.wetpaintserv.us/wiki/wikiradiography/widget/youtubevideo/931dd550c878e17f48c9b80af2d27f80336fa8a8" type="application/x-shockwave-flash" width="425" wmode="transparent"/> This is a basic video that explains consolidation in simple terms
Notes
- Consolidation may be complete or incomplete
- The distribution of the consolidation can vary widely.
- A consolidation could be described as “patchy”, “homogenous”, or generalised”.
- A consolidation may be described as focal or by the lobe or segment of lobe affected
Sutton, Textbook of Radiology, 2nd ed.,1975, p325
Interstitial vs Alveolar Patterns
Recognition of a plain film interstitial pattern is important because it identifies the abnormal density as being within the supporting tissues of the lung rather than within the air spaces, pleural space, mediastinum, or outside the thoracic cavity- it indicates the infiltrate's cellular rather than fluid nature.
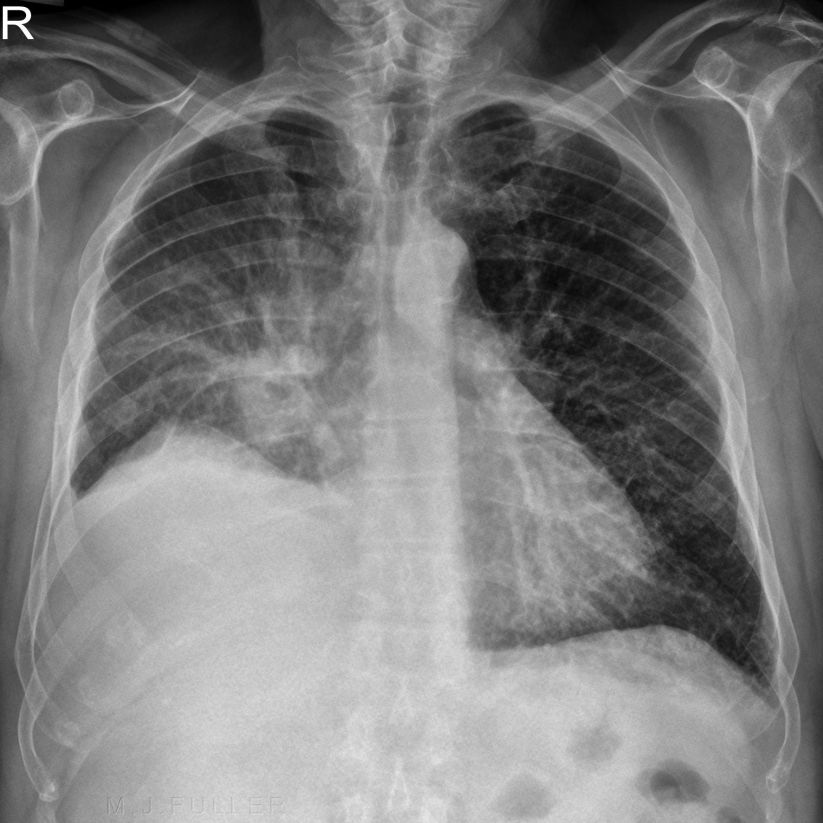
Alveolar Lung Patterns on CXR
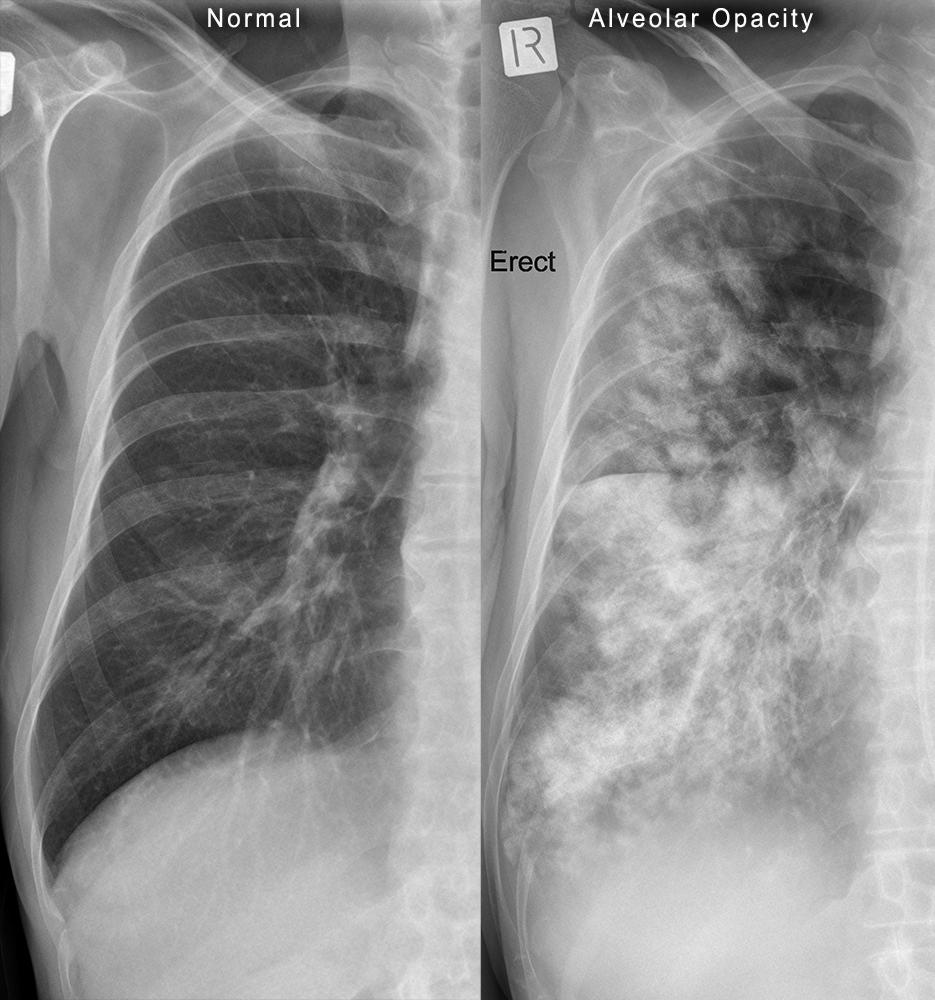
Alveolar Opacity Interstitial Opacity Alveolar Opacity- Definition Alveolar opacity refers to opacity on chest X-ray associated with fluid filling of the airspaces.
Interstitial Opacity- Definition The interstitium refers to the supporting structures of the lung. An interstitial opacity on chest X-ray refers to an abnormal appearance of the lung interstitium
Alveolar Opacity- Anatomy
<a class="external" href="http://www.ichristianschool.org/anatomy/3rdQuarter/anatomy23.htm" rel="nofollow" target="_blank">http://www.ichristianschool.org/anatomy/3rdQuarter/anatomy23.htm</a>Interstitial Opacity- Anatomy <a class="external" href="http://www.msdlatinamerica.com/ebooks/HighResolutionCToftheLung/sid129911.html" rel="nofollow" target="_blank">High-Resolution CT of the Lung, 3rd Edition, 2001 Lippincott Williams & Wilkins </a>
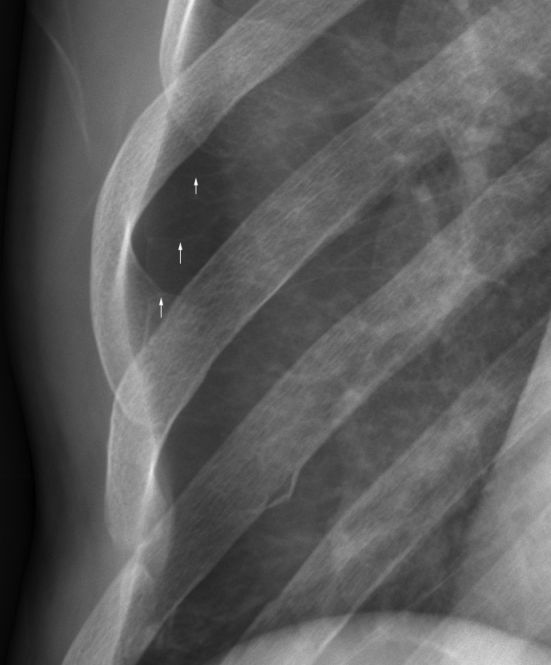
Well demonstrated normal interlobular septa in patient with pneumothorax
(pneumothorax causes alveolar compression and so, the intersitium forms a larger component of the lung volume).
Alveolar Opacity- Plain Film Pattern Interstitial Opacity- Plain Film Pattern
Alveolar pattern results from flooding of the end air spaces (acini) with fluid (pus, blood, edema) only rarely with cellular material. As individual acini become filled the fluid spreads to adjacent ones through the interalveolar pores. This results in the typical radiographic pattern of a poorly margined ("fluffy") density. The densities may spread and their borders coalesce. This may progress until all acini within a lung lobe are filled. There may be a sharp border at the edge of a lung lobe due to the pleura blocking further spread of the fluid into the adjacent lung lobe. As the number of fluid filled adjacent acini increases, the air filled, large and medium sized bronchi become evident as linear radiolucent branching structures (air bronchogram). The air-filled bronchi are surrounded by a fluid density and the bronchial wall and adjacent vessel are not seen. When a bronchus branches perpendicular to the x-ray beam it will be seen as a round radiolucent dot.
<a class="external" href="http://www.vin.com/proceedings/Proceedings.plx?CID=WSAVA2002&PID=2602" rel="nofollow" target="_blank">Radiographic Diagnosis of Pulmonary Disease</a><a class="external" href="http://www.vin.com/proceedings/Proceedings.plx?CID=WSAVA2002&PID=2602" rel="nofollow" target="_blank">Norman Ackerman, DVM, DACVR</a>
Interstitial Lung Patterns on CXR
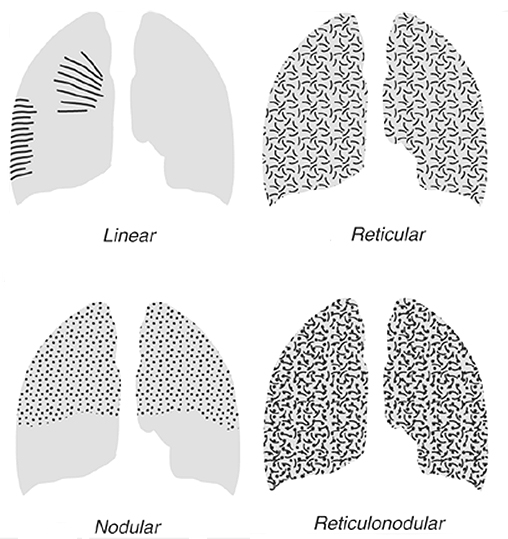
<a class="external" href="http://cox-radiology.org/content/e1653/e1451/e1851/approach-to-interstitial-lung-diseases.ppt" rel="nofollow" target="_blank">Pracical Approach to Interstitial Lung Diseases, A. Nour-Eldin</a>There are 4 basic interstitial lung patterns
- linear- septal lines (Kerley lines)
- reticular- mesh like appearance, lines in all directions
- nodular- discrete opacities
- reticulonodular- combination of 2 and 3
Linear Interstitial Pattern
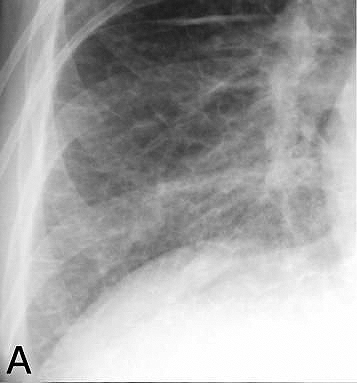
This is a fine linear interstitial patternReticular Interstitial Pattern Nodular Interstitial Pattern This is a nodular pattern in a patient with lymphangitis carcinomatosis.
Reticulonodular Interstitial Pattern Reticulonodular pattern in a patient with COPD
The linear pattern on chest radiography consists of thin linear opacities which are either 2 to 6 cm long within the lungs oriented radially toward the hila or 1 to 2 cm long at right angles to, and in contact with, the lateral pleural surfaces. These linear opacities have been referred to as Kerley A and Kerley B lines, respectively, although the descriptors “septal thickening” or “septal lines” are now preferred for the latter.
Histologically, this linear pattern represents thickening of either the bronchovascular/axial interstitium (Kerley A) or the peripheral interstitium (Kerley B).The linear opacities may be single or multiple, regional or diffuse, and short or long, depending on the etiology and severity of disease.
The most common cause of the linear pattern is hydrostatic pulmonary edema, but other etiologies include lymphangitic carcinomatosis, and atypical interstitial pneumonias such as those caused bymycoplasma, chlamydia, cytomegalovirus (CMV), and respiratory syncytial virus (RSV). Interstitial pulmonary edema tends to be symmetric in distribution while atypical infections and lymphangitic carcinomatosis may be asymmetrical.
<a class="external" href="http://www.appliedradiology.com/Issues/2009/12/Articles/Revisiting-the-pattern-approach-to-interstitial-lung-disease-on-chest-radio/Revisiting-the-pattern-approach-to-interstitial-lung-disease-on-chest-radiography.aspx" rel="nofollow" target="_blank">Scott D. Perrin, MD, Adam Ulano, MD, and Todd R. Hazelton, MD
Revisiting the pattern approach to interstitial lung disease on chest radiography
Aplied Radiology
Volume 38, Number 12, December 2009</a>
The reticular pattern as seen on chest radiography and computed tomography (CT or HRCT) is depicted by numerous, small, linear opacities which, by summation, have been described as a lace-like or net-like in appearance.4,5 The reticular pattern can be divided into 3 distinct groups, each of which suggests different diagnoses: peripheral reticular pattern with small lung volumes, diffuse reticular/cystic pattern with normal or increased lung volumes, and airway/central reticular pattern.
<a class="external" href="http://www.appliedradiology.com/Issues/2009/12/Articles/Revisiting-the-pattern-approach-to-interstitial-lung-disease-on-chest-radio/Revisiting-the-pattern-approach-to-interstitial-lung-disease-on-chest-radiography.aspx" rel="nofollow" target="_blank">Scott D. Perrin, MD, Adam Ulano, MD, and Todd R. Hazelton, MD
Revisiting the pattern approach to interstitial lung disease on chest radiography
Aplied Radiology
Volume 38, Number 12, December 2009</a>
<a class="external" href="http://www.appliedradiology.com/Issues/2009/12/Articles/Revisiting-the-pattern-approach-to-interstitial-lung-disease-on-chest-radio/Revisiting-the-pattern-approach-to-interstitial-lung-disease-on-chest-radiography.aspx" rel="nofollow" target="_blank">Scott D. Perrin, MD, Adam Ulano, MD, and Todd R. Hazelton, MD
Revisiting the pattern approach to interstitial lung disease on chest radiography
Aplied Radiology
Volume 38, Number 12, December 2009</a>
1. Linear
A linear pattern is seen when there is thickening of the interlobular septa, producing Kerley lines
The most common cause of interlobular septal thickening, producing Kerley A and B lines, is pulmonary edema
other causes
- Mitral stenosis
- Lymphangitic carcinomatosis
- Malignant lymphoma
- Idiopathic pulmonary fibrosis
- Pneumoconiosis
- Sarcoidosis
Note the obscuration of the normal lung markings in the patient with the linear interstitial pattern
2. Reticular
A reticular pattern results from the summation or superimposition of irregular linear opacities. The term reticular is defined as meshed, or in the form of a network. Reticular opacities can be
described as fine, medium, or coarse, as the width of the opacities increases. A classic reticular pattern is seen with pulmonary fibrosis, in which multiple curvilinear opacities form small cystic spaces along the pleural margins and lung bases (honeycomb lung)
3. Nodular
4. Reticulonodular
Distinguishing Acinar nodules from from interstitial nodules
Acinar
- Varying in size
- Indistinct edges
- Larger than interstitial nodules
Interstitial
- Same size
- Sharp edges
- smaller
... back to the Wikiradiography home page
... back to the Applied Radiography home page