Foreign Body Radiography
Jump to navigation
Jump to search
Introduction
Mechanisms
Radiography
Self-adhesive Foreign Body Markers
Case 1
Case 2
Case 3
Case 4
... back to the Applied Radiography home page
... back to the Wikiradiography home page
Relevant Wiki PagesRadiography for suspected foreign body is a commonplace radiographic examination. This page considers all aspects of radiography for suspected foreign body.
Radiography for Ingested/Aspirated Foreign Bodies
Chest Radiography for Inhaled Foreign Body
Imaging Nail Gun Injuries
Lateral Soft Tissue Neck for Foreign Body
Mechanisms
- accidental
- intentional
- iatrogenic.
Radiography
Radiographers will usually start with conventional orthogonal views- e.g. AP and lateral. The images are reviewed to assess the potential value of supplementary views. The following should be noted;
- at least one joint should be included with longbone projections whenever possible
- the foreign body may not be near the entry site- don't collimate the beam too tightly
- centring the X-ray beam on the likely position of the foreign body will reduce parallax error
- an entry site marker provides a useful guide to the position of the foreign body relative to the entry site
- ensure that the entry site marker is not confused with the foreign body
- it is possible for an entry site marker to obscure a small foreign body
- a tangential view of the foreign body can be useful for demonstrating the depth of the foreign body below the skin
- it can be useful to image the foreign body separately if the patient has provided an example of the same item
- when using film/screen, a soft tissue exposure may be appropriate
- where there are multiple possible entry sites, it may be useful to leave the entry site marker in place for the surgeon to see.
Self-adhesive Foreign Body Markers
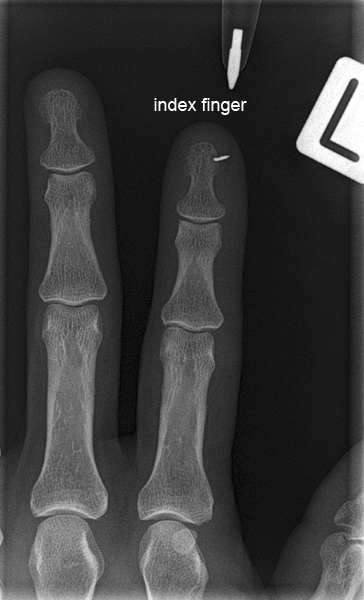
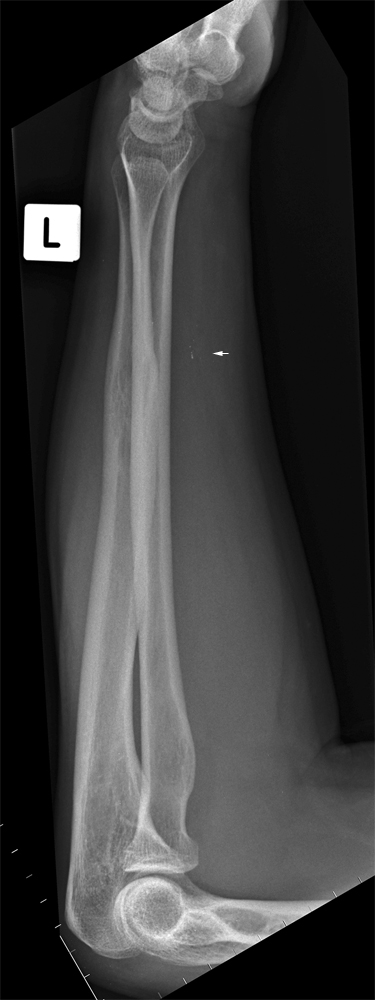
Case 1
This patient presented to the Emergency Department after an incident in which a fragment of ferrous metal casting was suspected to have lodged in his upper arm. The patient (with admirable ingenuity) found a rare earth magnet and placed it against his skin where he thought the foreign body was sited. The magnet adhered to his arm. When the magnet approached the patient's arm over the site of the suspected foreign body, the patient could feel the pull on the magnet under his skin. When the magnet was pulled away from his arm, the skin tented with the magnetic attraction to the foreign body under his skin. The patient was referred for radiography of his upper arm to confirm the size and location of the foreign body.
Note the dried blood at the entry sire.Conventional AP and lateral views of the humerus/elbow were obtained. The entry site was marked by placing an ink pen (biro) on the cassette that lined up with the entry site. This method has the advantage of being quick and easy to execute and the disadvantage of often only being achievable on one view (when the entry site is in contact with the cassette, it is not visible and therefore cannot be marked). An alternative method is to use a commercial adhesive disposable lead (pb) marker. This method has the advantage of providing an entry site identification which is visible on all views. It has the disadvantage of providing an opaque marker that can be confused with the foreign body(s). In addition, it may not always be practicable to adhere anything to the entry site. Entry site marking largely becomes a question of judgement; where the foreign body will be removed under image intensifier control, the entry site marker is somewhat redundant. Where the foreign body is known and will not be confused with the entry site marker (most cases) and the entry site is suitable for an adhesive commercial entry site marker, this is a good choice.
The imaging demonstrates a small metallic foreign body (arrow). An additional tangential view to show the depth of the foreign body was considered unnecessary given that tenting of the patient's skin when a magnet was applied.
There is benefit in centring the X-ray beam to the foreign body to avoid parallax error.The tip of an ink pen provides a handy entry point marker.
The practice of using an unfolded pair of paper clips to mark the entry site is arguably effective but aesthetically woeful.
Case 2
Case 3
Case 4
... back to the Applied Radiography home page
... back to the Wikiradiography home page