CT Case 3 - Subarachnoid Haemorrhage with Cerebrovascular Spasm
Jump to navigation
Jump to search
Introduction
A head CT and CTA were performed on a 34 year old female with acute cardiorespiratory arrest, dilated unresponsive pupils, and GCS 3.
Results
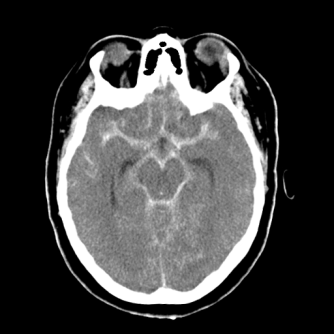
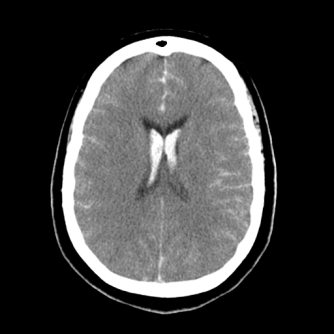
On the pre-contrast head CT there is extensive acute subarachnoid haemorrhage (SAH) present as seen on Image A and B below.
Image A Extensive acute subarachnoid haemorrhage within the subarachnoid cisterns.
Image B Acute subarachnoid haemorrhage extending into the lateral ventricles, falx cerebri, and sulci.
The CTA of the Circle of Willis, and the carotid and vertebral arteries, demonstrates opacification of the carotid arteries in the neck and in the vertebrobasilar arteries. However, the intracranial branches of the carotids, the distal right internal carotid, and the basilar artery are not opacified (See Image C). This is most likely due to severe cerebrovascular spasm. There is an 8×4mm elongated aneurysm on the left vertebral artery within the foramen magnum and could possibly be the cause of the SAH (See Image D).

Image C Contrast visualised in the vertebrobasilar arteries but not in the intracranial arteries due to severe vascular spasm.
Image D 3D image demonstrating an aneurysm of the left vertebral artery within the foramen magnum.
Discussion
Cerebrovascular spasm is a common complication of SAH and accounts for many of the associated deaths. It occurs in 20-50% of patients who have had an aneurysm rupture and usually occurs 3 to 14 days after the SAH. Cerebrovascular spasm is not always symptomatic but can result in symptomatic ischaemia and infarction in the territories that are supplied by those vessels affected. Cerebrovascular spasm is typically characterised by a decline in neurological status but it can be reversible and does not always indicate permanent brain injury. Subarachnoid blood is thought to cause spasm in the adjacent arteries due to the constrictive effects of platelet and red blood cell products. In this case cerebrovascular spasm occurred straight away due to the extensive SAH and the patient was given a very poor prognosis and was later determined brain dead.
References
Chandy, D, Sy, R, Aronow, W, Lee, W, Maguire, G & Murali, R (2006) ‘Hyponatremia and cerebrovascular spasm in aneurysmal subarachnoid hemorrhage’, Neurology India, Vol. 54, pp. 273-275.
Chapman, S & Nankielny, R (2003) ‘Aids to radiological differential diagnosis’, 4th edn, Saunders, Edinburgh.
Kumar, V, Cotran, R & Robbins, S (1992) ‘Basic pathology’, 5th edn, WB Saunders Company, Philadelphia.
Weir, J & Murray, A (1998) ‘Mosby’s atlas and text of clinical imaging’, Mosby-Wolfe, London.